Overview
This article highlights the secondary conditions associated with PTSD that veterans should be aware of, including:
- Migraines
- Sleep apnea
- Gastrointestinal issues
- Cardiovascular diseases
We understand that recognizing these conditions is crucial for effective management and benefits claims. Many veterans face significant health challenges related to their trauma, which can complicate their pursuit of necessary support and resources.
It's common to feel overwhelmed by these additional health concerns. By acknowledging these issues, veterans can take proactive steps toward better health. Remember, you are not alone in this journey; we’re here to help you navigate these challenges and find the support you need.
Understanding the connection between PTSD and these secondary conditions can empower veterans to seek the care they deserve. Together, we can work towards a healthier future.
Introduction
Understanding the complex landscape of post-traumatic stress disorder (PTSD) reveals that its impact extends far beyond mental health. We recognize that many veterans face a range of secondary conditions, such as:
- Migraines
- Sleep apnea
- Chronic pain
- Cardiovascular issues
These interconnected health challenges can complicate lives, posing significant barriers to well-being and access to necessary support.
This article delves into ten critical PTSD secondary conditions, highlighting their implications for veterans. It's essential to understand that you're not alone in facing these hidden struggles. Comprehensive advocacy plays a crucial role in navigating the often-overwhelming benefits system.
How can former service members effectively address these challenges and secure the assistance they deserve? Together, we can explore the paths to support and healing.
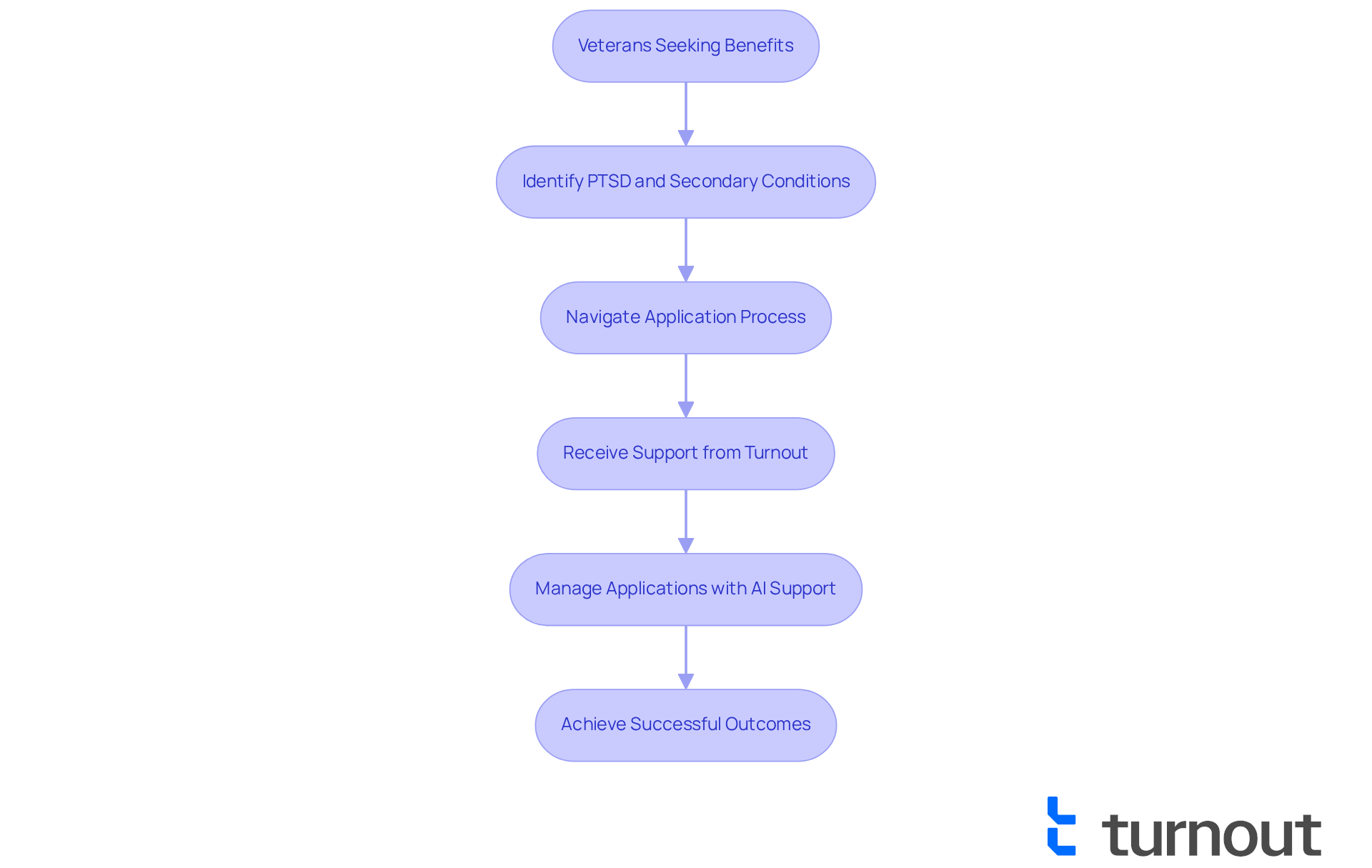
Turnout: Advocacy for Veterans Navigating PTSD Secondary Conditions
Turnout is dedicated to supporting former service members as they navigate the challenges of trauma and the associated PTSD secondary conditions. We understand that the journey can be overwhelming, but by utilizing technology and empathetic support, Turnout ensures that former service members obtain the benefits and assistance they deserve. This advocacy is essential, particularly as many former military personnel face bureaucratic hurdles when pursuing support for issues associated with their service-related trauma.
The effects of post-traumatic stress disorder on former military personnel extend beyond mental well-being. They frequently result in additional issues such as diabetes, erectile dysfunction (ED), and gastroesophageal reflux disease (GERD). These circumstances can complicate the benefits application process, making it even harder for former service members to receive the assistance they need. Studies show that those with trauma-related disorders face a significantly heightened risk for various health complications, including cardiovascular issues, which can further impede their ability to manage the benefits system efficiently.
Veterans supporters stress the importance of understanding PTSD secondary conditions when seeking benefits. It's common to feel uncertain about eligibility, especially regarding PTSD secondary conditions that arise from trauma. This lack of awareness can lead to missed opportunities for support and resources, which is why we are here to help.
Turnout addresses these challenges directly by providing a streamlined approach to benefits navigation. With the help of Jake, the AI case quarterback, service members can easily manage their applications, stay updated on deadlines, and receive proactive follow-ups. This innovative model not only alleviates the stress associated with the application process but also enhances the likelihood of successful outcomes.
Recent advancements in support for those with trauma have underscored the need for thorough advocacy. Initiatives focused on enhancing the availability of mental wellness services and tackling the stigma surrounding trauma are gaining momentum. Turnout is at the forefront of these efforts, advocating for policies that prioritize the mental health needs of former military personnel and ensuring they receive the benefits they have earned.
Effective consumer advocacy for former military personnel experiencing trauma is crucial in transforming the landscape of support services. By concentrating on the unique challenges faced by former service members, Turnout is helping to create a more accessible and compassionate system. This enables individuals to reclaim their lives and navigate the complexities of their benefits with confidence. Remember, you are not alone in this journey—we're here to support you every step of the way.
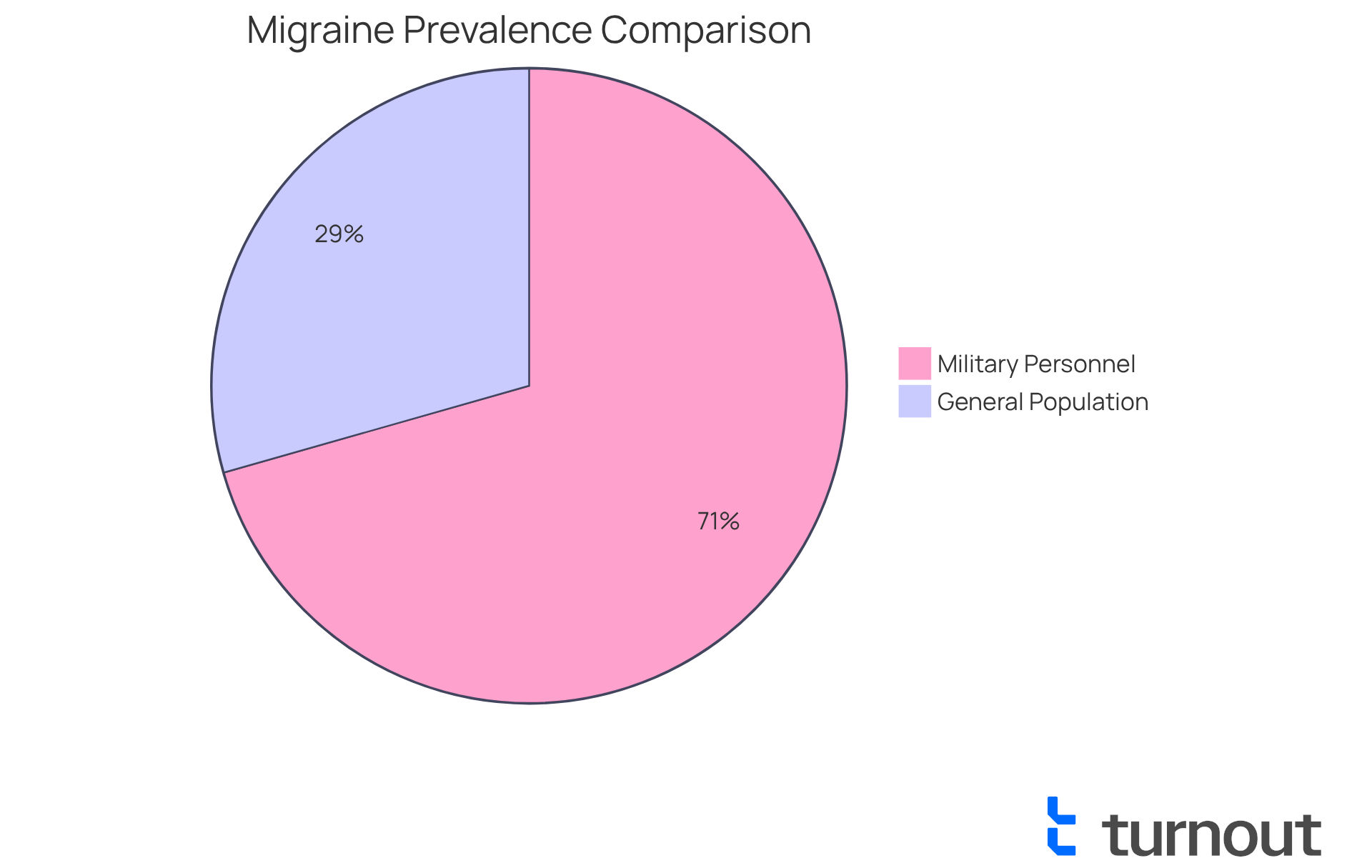
Migraines: A Common Secondary Condition Linked to PTSD
Migraines can be a significant issue for those dealing with trauma-related stress and PTSD secondary conditions. We understand that the stress and anxiety linked to PTSD can trigger migraine episodes, leading to debilitating pain and discomfort. Research indicates that up to 36% of individuals who served during Operation Enduring Freedom/Operation Iraqi Freedom suffer from migraines, compared to just 12% to 15% of the general population. This stark difference highlights the importance of tracking your symptoms and seeking medical evaluation if you experience frequent migraines.
Establishing a connection between migraines and PTSD secondary conditions is vital for accessing potential disability benefits. Often, this requires a nexus letter and supporting medical documentation. The VA evaluates the severity of migraines based on their impact on daily life and work, commonly assigning ratings of:
- 30% for moderate impairment
- 50% for severe impairment
Understanding how PTSD secondary conditions can lead to migraines—through heightened stress, anxiety, and sleep disturbances—can empower former military personnel to manage their symptoms and advocate for their rights to benefits. We encourage you to consult with qualified medical professionals who can assist in creating a nexus letter, significantly improving your chances of a successful claim. Remember, you are not alone in this journey, and we’re here to help you navigate these challenges.
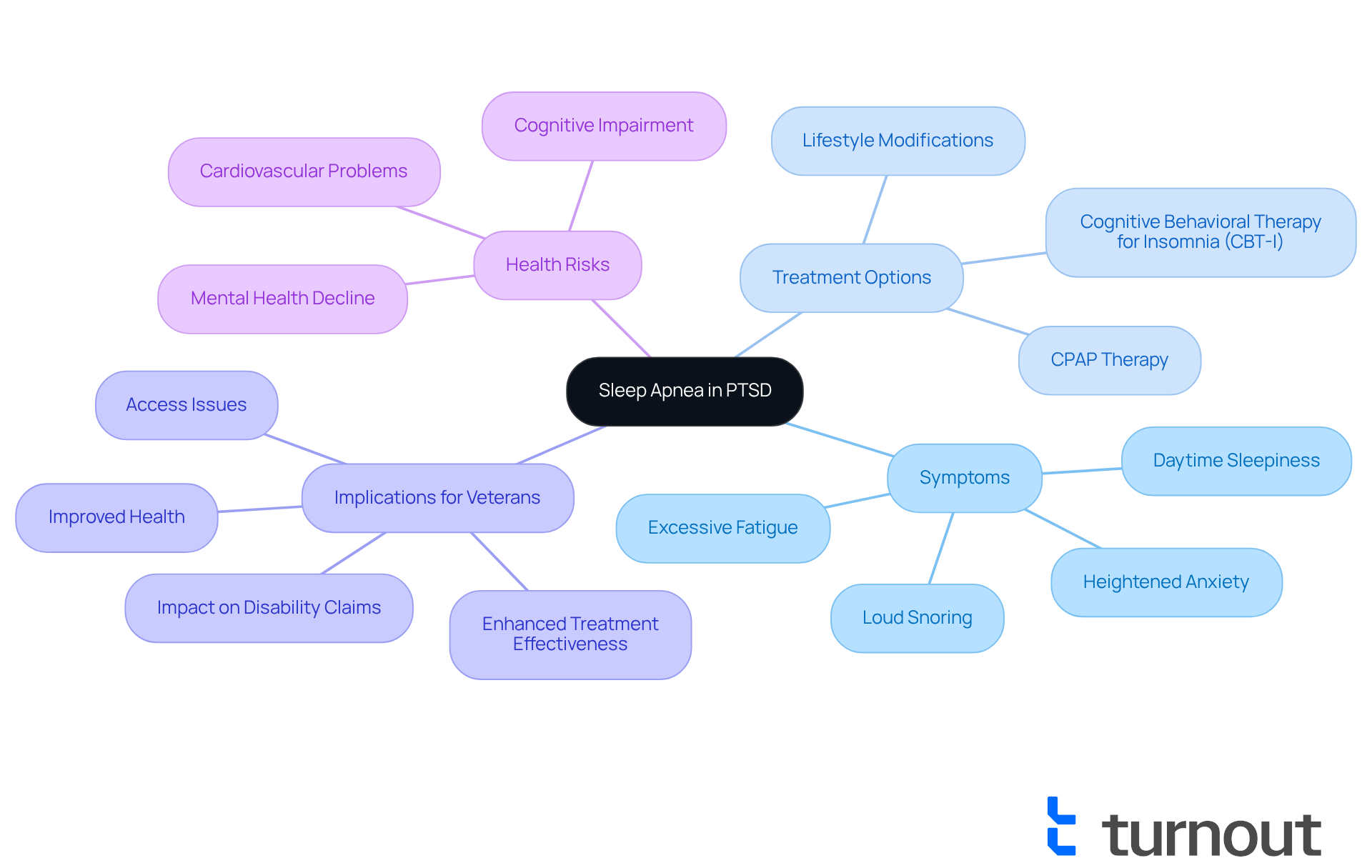
Sleep Apnea: A Notable Secondary Condition of PTSD
Sleep apnea is a condition that many former military personnel face, especially those dealing with trauma-related stress. This condition can disrupt sleep patterns, leading to increased fatigue and heightened anxiety, which complicates the management of PTSD secondary conditions. It's essential for veterans to be vigilant for signs of sleep apnea, such as loud snoring and excessive daytime sleepiness. Seeking medical evaluation can open doors to effective treatment options. Managing sleep apnea not only enhances overall health but may also strengthen claims for disability benefits. Untreated sleep apnea can adversely affect disability compensation for former service members.
Experts stress the importance of addressing sleep issues in veterans who are facing PTSD secondary conditions. Dr. Mark Gladwin emphasizes, "Providing CPAP treatment can significantly reduce the risk of dying from heart-related causes by 55% and from any cause by 37%." Furthermore, research indicates that individuals with severe trauma-related symptoms, which can include PTSD secondary conditions, are at a considerably increased risk for sleep apnea. In fact, nearly 70% of young service members in one study were identified as high risk for this condition.
Treatment options for sleep apnea include:
- Continuous Positive Airway Pressure (CPAP) therapy
- Lifestyle modifications
- Cognitive Behavioral Therapy for Insomnia (CBT-I)
These interventions can greatly improve sleep quality and overall mental well-being, potentially lowering the risk of cardiovascular problems associated with untreated sleep apnea.
Addressing sleep apnea is crucial for former service members to prevent PTSD secondary conditions. It can enhance the effectiveness of trauma treatments and improve their quality of life. Unfortunately, the lack of sleep specialists in the military can hinder access to essential care. Therefore, it's even more important for veterans to recognize and tackle this secondary condition, taking proactive steps toward better health and well-being. Remember, you are not alone in this journey, and we're here to help.
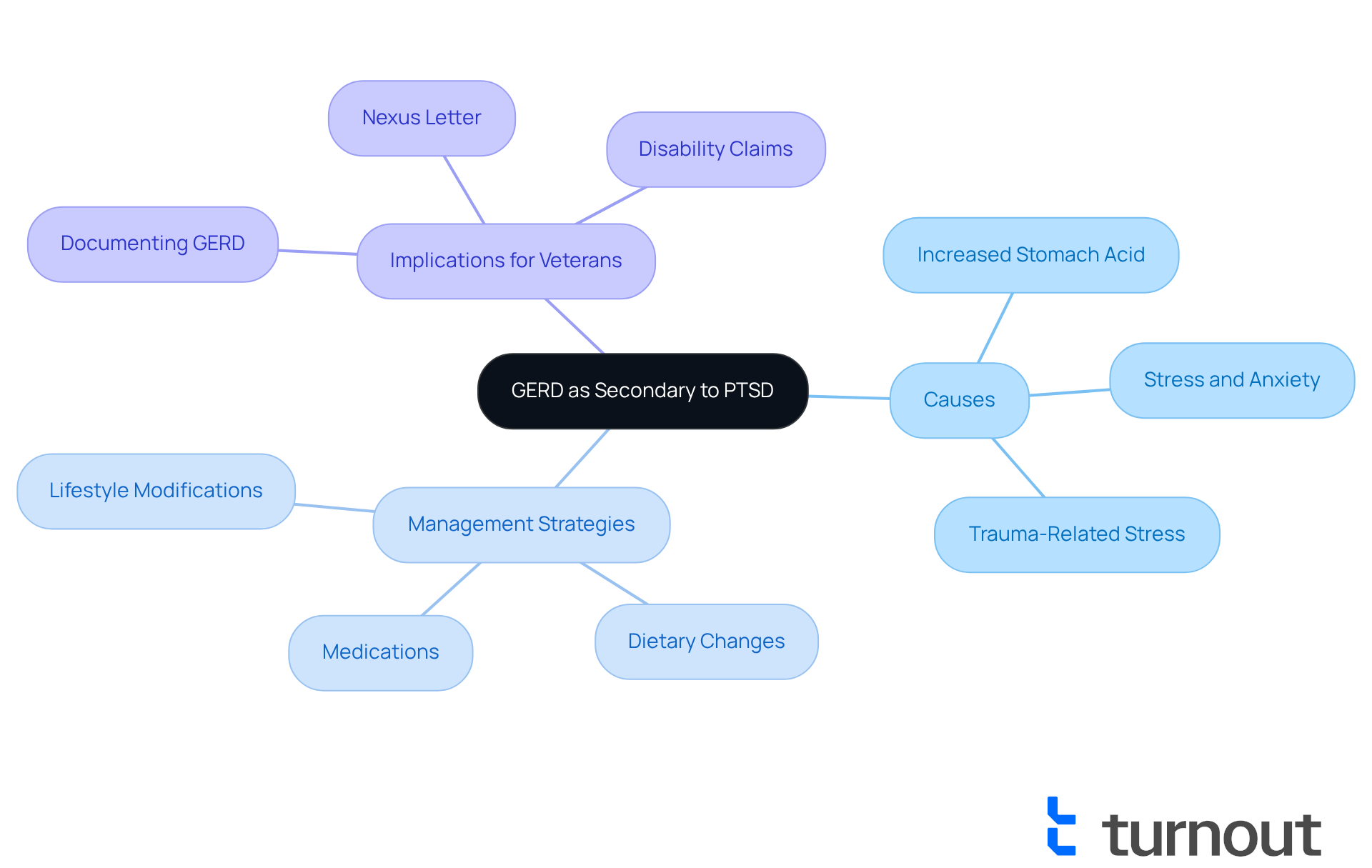
Gastroesophageal Reflux Disease (GERD): Secondary to PTSD
Gastroesophageal reflux disease (GERD) is a common concern for individuals diagnosed with post-traumatic stress disorder (PTSD). We understand that the heightened stress and anxiety associated with PTSD can lead to increased stomach acid production, which may worsen GERD symptoms. Research indicates that former service members experiencing trauma-related stress are significantly more likely to face gastrointestinal issues, with studies showing they are twice as likely to develop such conditions compared to their peers without similar stress. This connection highlights the importance of recognizing GERD as a potential secondary issue linked to trauma-related stress and PTSD secondary conditions.
If you're a veteran dealing with GERD, it’s crucial to consult with healthcare providers for effective management strategies. Gastroenterologists recommend a comprehensive approach to treatment, which may include:
- Lifestyle modifications
- Dietary changes
- Medication to help control symptoms
Additionally, it’s essential for former military personnel to document their GERD condition. Demonstrating a connection between GERD and trauma, especially regarding PTSD secondary conditions, can be vital for disability claims. Having proper medical evidence, such as a diagnosis of GERD and a nexus letter from a physician, can strengthen claims for PTSD secondary conditions in relation to secondary service connection. This may lead to increased VA disability ratings and additional compensation.
You are not alone in this journey, and support is available to help you navigate these challenges. We’re here to help you find the right path to managing your health.
Irritable Bowel Syndrome (IBS): A Secondary Condition Associated with PTSD
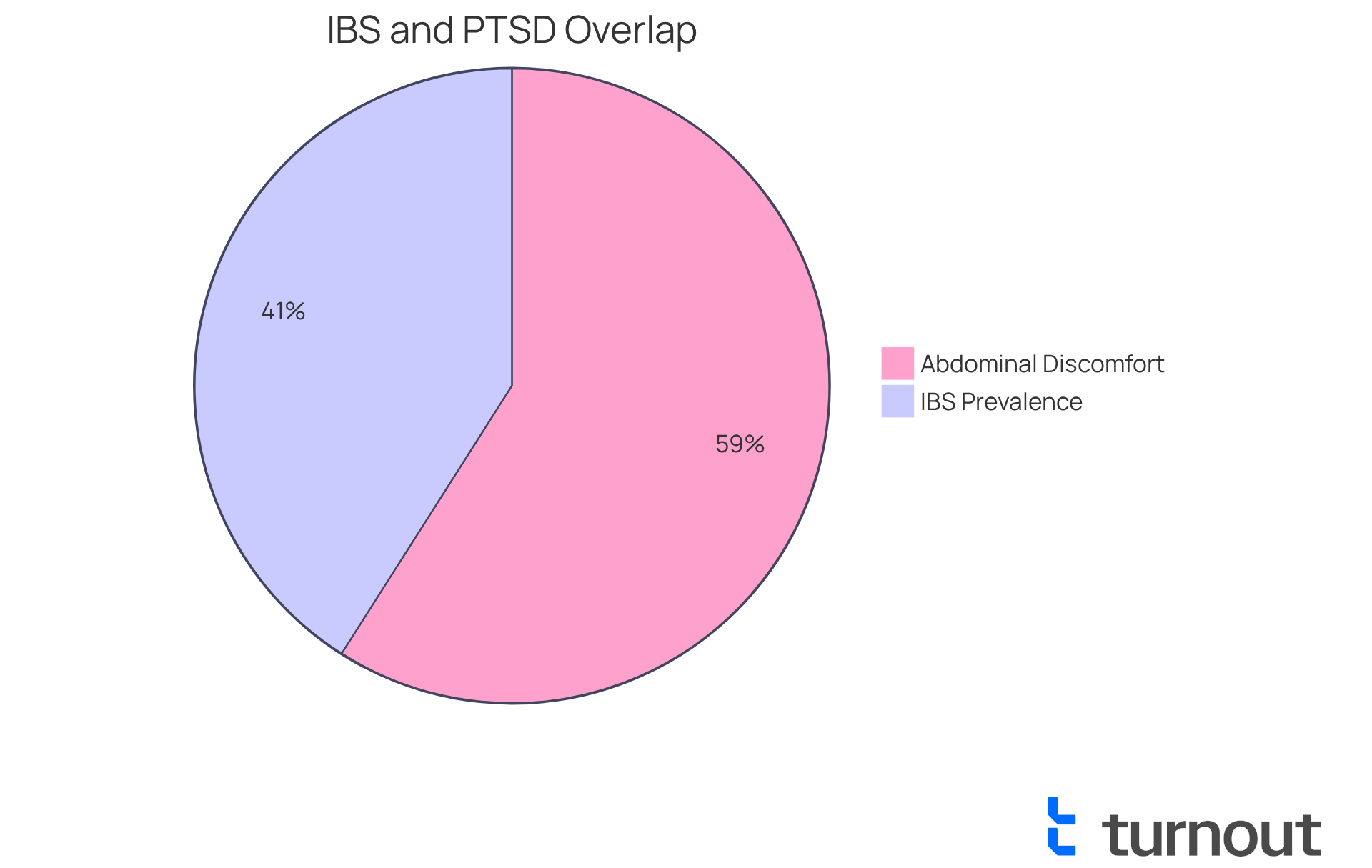
Irritable bowel syndrome (IBS) is a common gastrointestinal condition that affects many former military personnel dealing with trauma-related stress. We understand that the stress response associated with post-traumatic stress disorder (PTSD) can significantly disrupt normal gastrointestinal function, potentially resulting in PTSD secondary conditions. This disruption often leads to uncomfortable symptoms such as abdominal pain, diarrhea, constipation, and bloating. Studies reveal that approximately 25% of military personnel with trauma disorders meet the criteria for IBS, a rate that is notably higher than in the general population. It's concerning to note that 36% of individuals with PTSD secondary conditions report symptoms like abdominal discomfort, highlighting the widespread nature of these issues.
Healthcare providers emphasize the importance of discussing any gastrointestinal symptoms with medical professionals. It’s common to feel overwhelmed, but specialists remind us that ongoing stress and hyperarousal from trauma exposure can trigger gastrointestinal symptoms, including IBS, which often lack identifiable physical causes. Addressing these symptoms effectively is essential, as it can enhance overall well-being and support individuals in their claims for disability benefits.
Veterans experiencing gastrointestinal issues should take the initiative to seek evaluations and appropriate referrals. Understanding the connection between PTSD and PTSD secondary conditions related to digestive health is crucial. By tackling these secondary issues, we can ensure that former service members receive the care and support they truly deserve. Remember, you're not alone in this journey, and we're here to help you navigate these challenges.
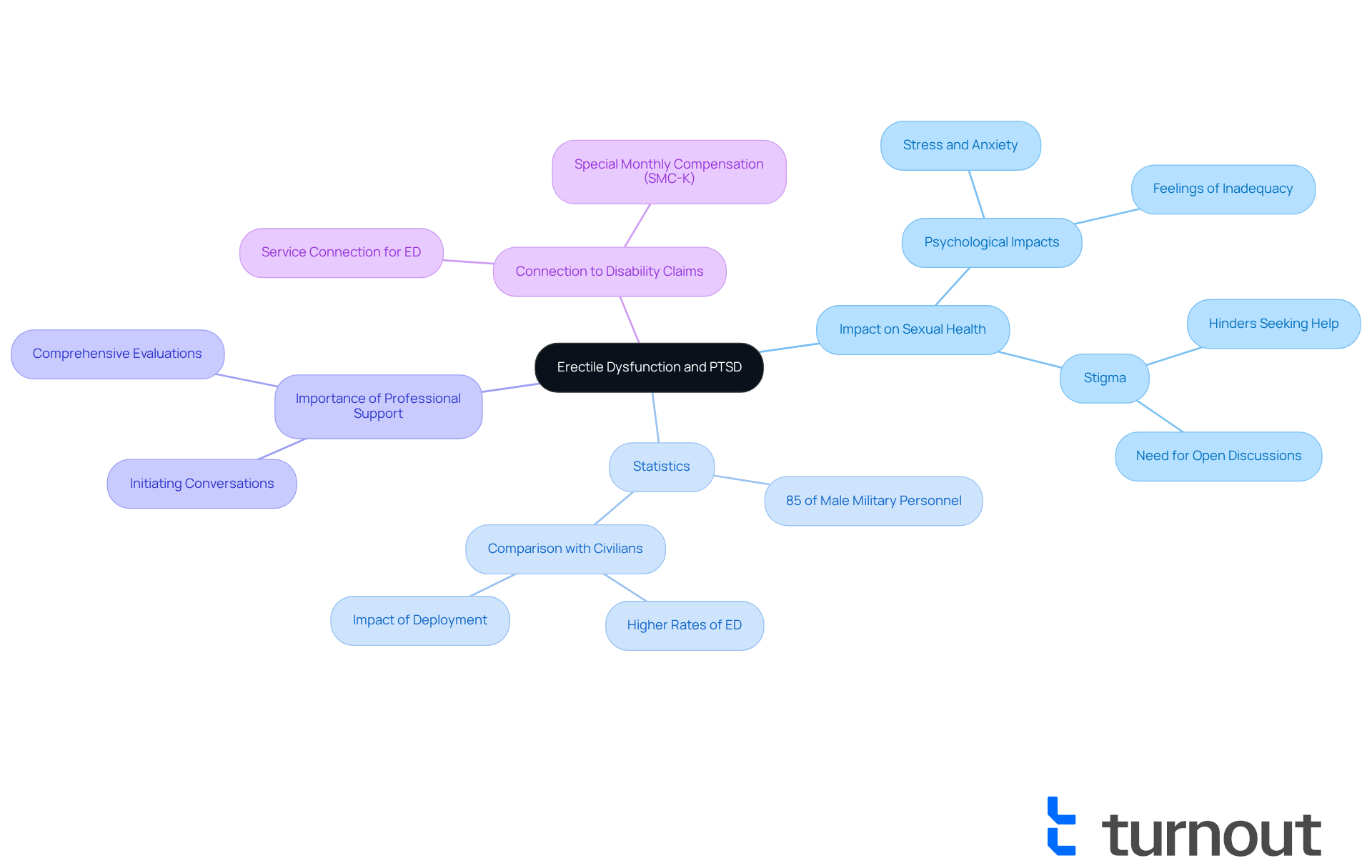
Erectile Dysfunction (ED): Impact of PTSD on Sexual Health
Erectile dysfunction (ED) is a common challenge for many individuals diagnosed with post-traumatic stress disorder (PTSD), often arising from the psychological impacts of trauma and classified as one of the PTSD secondary conditions. We understand that the stress and anxiety associated with PTSD secondary conditions can significantly affect sexual function, leading to feelings of inadequacy and frustration. In fact, studies reveal that around 85% of male military personnel suffering from trauma-related disorders report experiencing erectile dysfunction—this rate is nearly four times higher than that of their peers without psychological conditions. Such a striking statistic highlights the urgent need for awareness and effective treatment options. Furthermore, male veterans with PTSD are notably more likely to report erectile dysfunction or other sexual issues compared to their civilian counterparts.
Mental health professionals emphasize the importance of addressing sexual health as a vital component of overall well-being. It's common to feel that PTSD secondary conditions disrupt various aspects of sexual functioning, including desire, arousal, and satisfaction. Unfortunately, the stigma surrounding these concerns often hinders former service members from seeking help. However, many express that it would be easier to discuss these topics if their healthcare providers initiated the conversation. Open discussions led by healthcare professionals can lead to improved outcomes.
If you are a veteran experiencing ED, we encourage you to consult healthcare professionals for comprehensive evaluations and treatment options. These conversations are not only essential for your well-being but can also play a significant role in disability claims. Establishing a clear connection between PTSD, erectile dysfunction, and PTSD secondary conditions is crucial for former service members pursuing benefits. This connection may qualify you for additional compensation related to service-related issues, including Special Monthly Compensation (SMC-K) for the loss of use of a creative organ. By addressing these challenges, you can regain your quality of life and navigate the complexities of your health with renewed confidence.
Hypertension: A Common Secondary Condition Related to PTSD
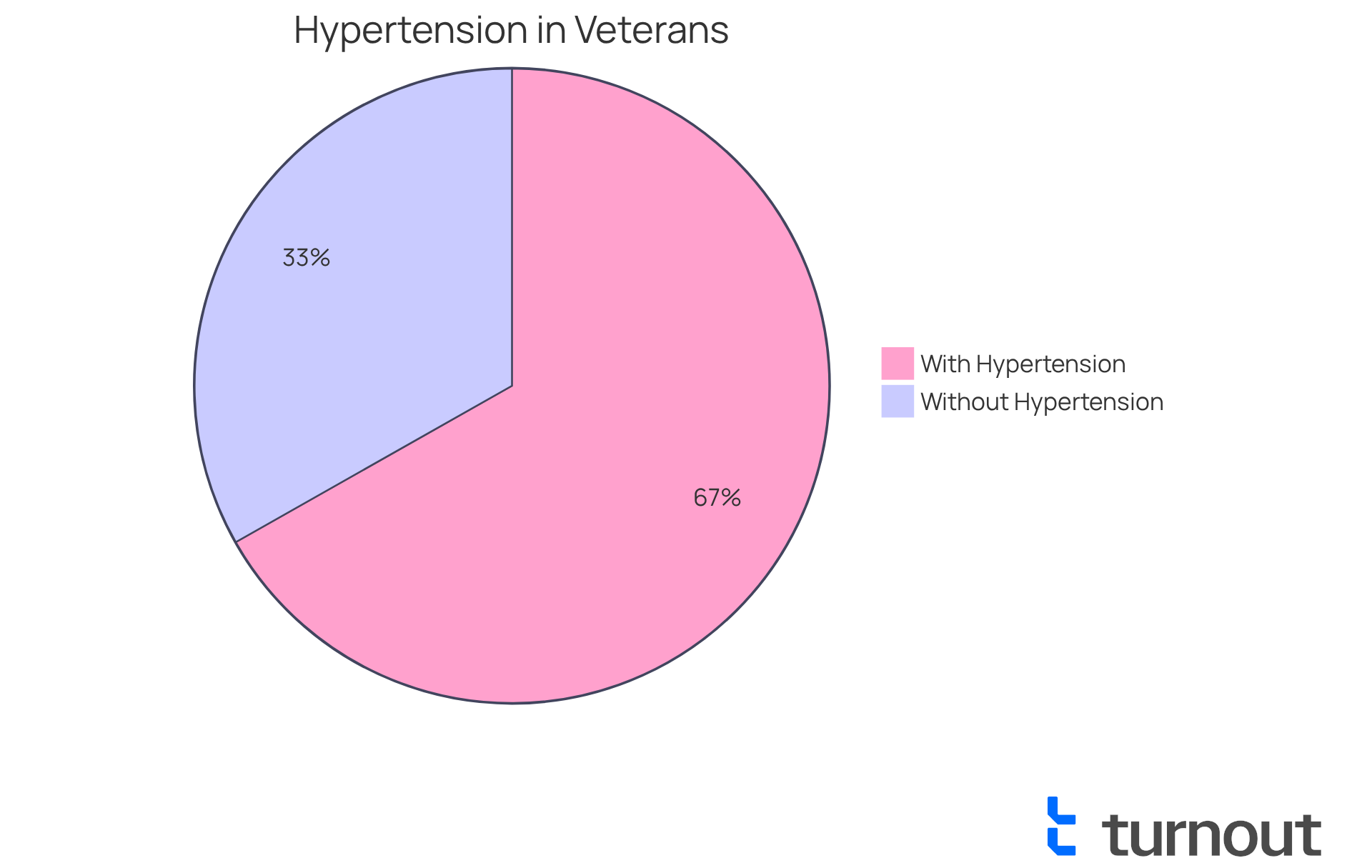
High blood pressure, or hypertension, is a common concern for many former military personnel who have PTSD secondary conditions. We understand that the persistent stress associated with PTSD secondary conditions can significantly elevate blood pressure levels, increasing the risk of cardiovascular complications. Studies reveal that male former service members facing trauma-related stress are 1.57 times more likely to experience hypertension when they have PTSD secondary conditions compared to those without such conditions. Alarmingly, 66.8% of these individuals exhibit high blood pressure.
This connection highlights the importance of regular blood pressure checks for former service members at risk of PTSD secondary conditions. Unmanaged hypertension can lead to serious medical issues, and cardiologists emphasize the need for tailored management strategies that address both psychological trauma and the PTSD secondary conditions it can cause. For instance, one cardiologist noted, "It is essential for former military personnel to participate in routine screenings and proactive management of their blood pressure to reduce long-term wellness risks."
We encourage veterans to seek guidance from healthcare professionals to develop effective strategies for controlling their blood pressure. This is especially important as hypertension may impact disability benefits related to their trauma-related diagnosis. Furthermore, younger individuals with PTSD secondary conditions should be assessed early for hypertension, as proactive health management can significantly improve outcomes. Remember, you are not alone in this journey, and we're here to help you navigate these challenges.
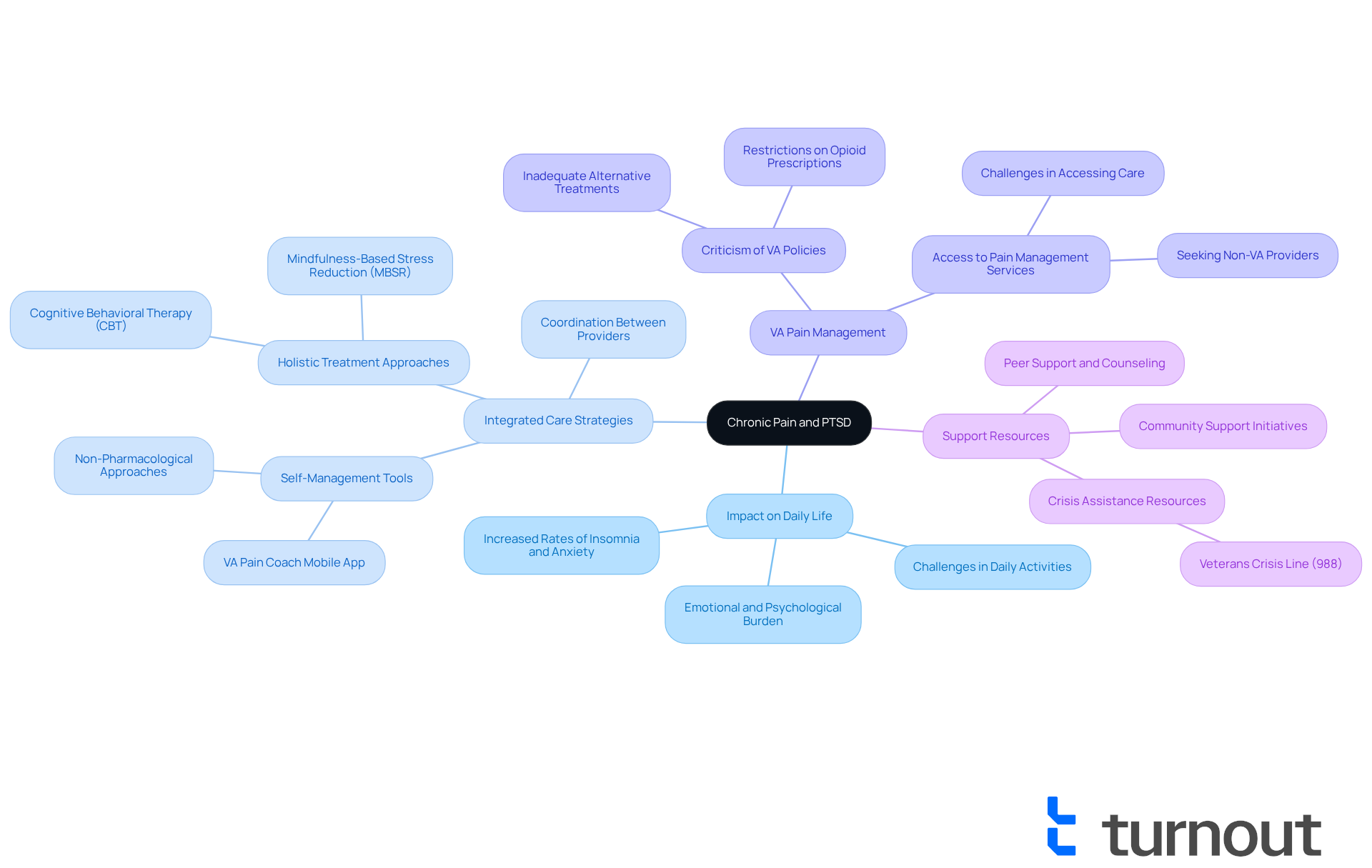
Chronic Pain: Secondary Condition Often Experienced by PTSD Sufferers
Chronic pain often emerges as a significant challenge for military personnel grappling with trauma-related disorders and PTSD secondary conditions. We understand that the intricate relationship between psychological trauma and physical pain can create a vicious cycle, where each condition worsens the other. Research indicates that around 50% of individuals with post-traumatic stress disorder also experience PTSD secondary conditions like chronic pain, which can greatly hinder their daily activities and overall health. This interplay highlights the importance of a comprehensive treatment strategy that addresses both PTSD and its secondary conditions, such as chronic pain, simultaneously.
By pursuing integrated care options, former service members can enhance their quality of life and strengthen their claims for disability benefits. Effective management of PTSD secondary conditions and other co-occurring conditions is crucial, as it not only alleviates suffering but also fosters a more supportive environment for recovery. However, it's common to feel overwhelmed when many former military personnel encounter difficulties in accessing sufficient pain management services, often prompting them to seek care beyond the VA system.
The VA's Pain Coach mobile app offers valuable resources for managing chronic pain, empowering veterans to take an active role in their treatment. Yet, we recognize that criticism of the VA's pain management policies highlights systemic issues that can hinder effective care. This underscores the need for a more compassionate and responsive approach to treatment. Remember, you are not alone in this journey; we’re here to help you navigate these challenges.
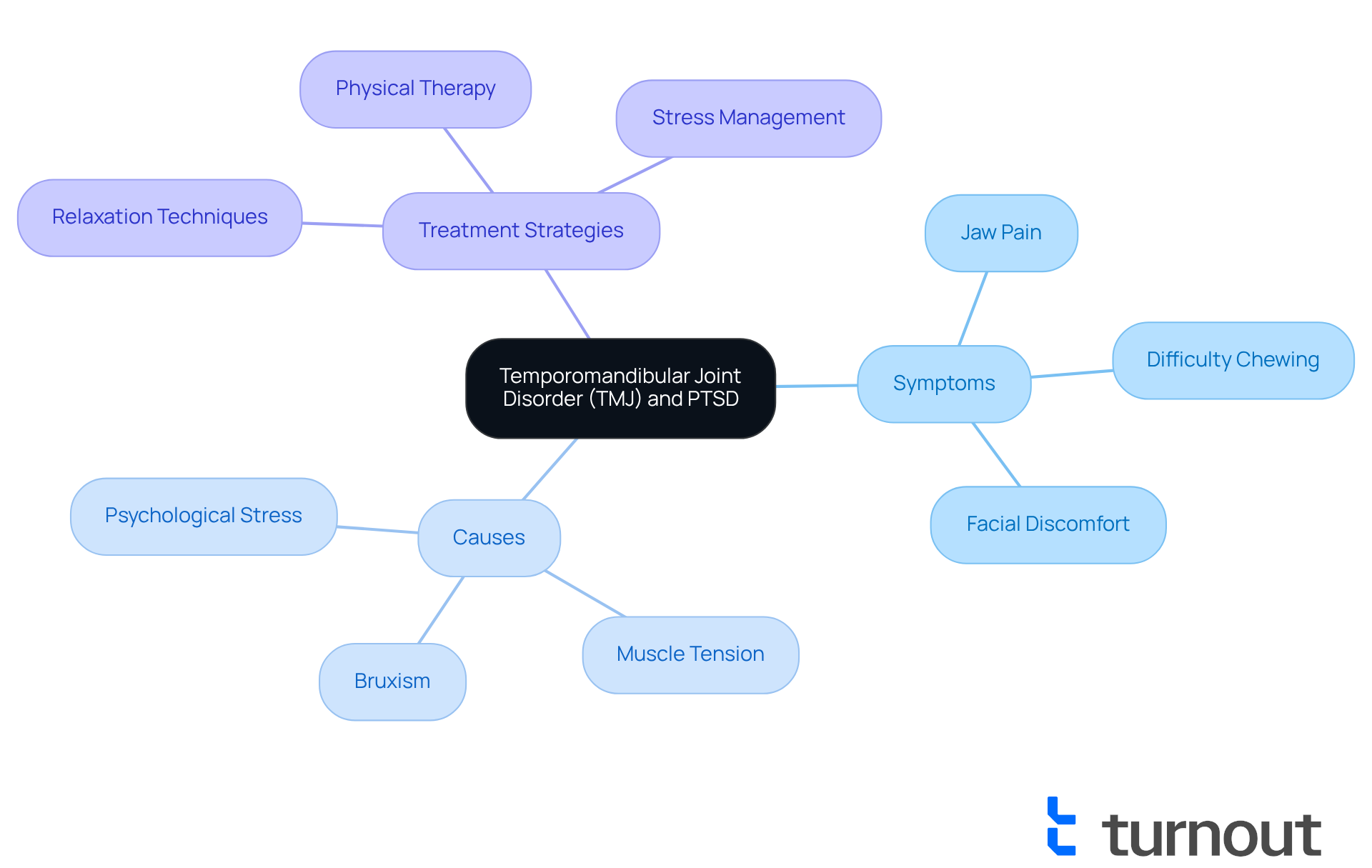
Temporomandibular Joint Disorder (TMJ): A Painful Secondary Condition of PTSD
Temporomandibular joint disorder (TMJ) is often linked with post-traumatic stress, manifesting through symptoms such as jaw pain, difficulty chewing, and facial discomfort. We understand that the psychological stress and anxiety resulting from PTSD secondary conditions can lead to increased muscle tension and bruxism, which in turn exacerbate TMJ issues. Research indicates that individuals diagnosed with PTSD secondary conditions exhibit a significantly higher prevalence of TMJ dysfunction. In fact, studies show that over 56% of war-exposed individuals present signs or symptoms of this disorder compared to non-exposed subjects.
Dental professionals highlight the significance of early assessment and treatment for those experiencing TMJ symptoms. Effective strategies may include:
- Relaxation techniques
- Physical therapy
- Stress management practices to alleviate muscle tension
As noted by Giuseppe Minervini, "Research has shown that war stress can be a major contributing factor to TMD." Furthermore, addressing TMJ issues is vital for former service members, as it can influence their disability claims, particularly regarding PTSD secondary conditions under the VA's evaluation standards detailed in 38 CFR 4.150 Schedule of Ratings. This highlights the need for comprehensive care that considers both physical and psychological health.
If you are experiencing TMJ symptoms, we encourage you to consult healthcare providers for tailored management plans that can improve your quality of life. Remember, you are not alone in this journey, and there are compassionate professionals ready to support you.
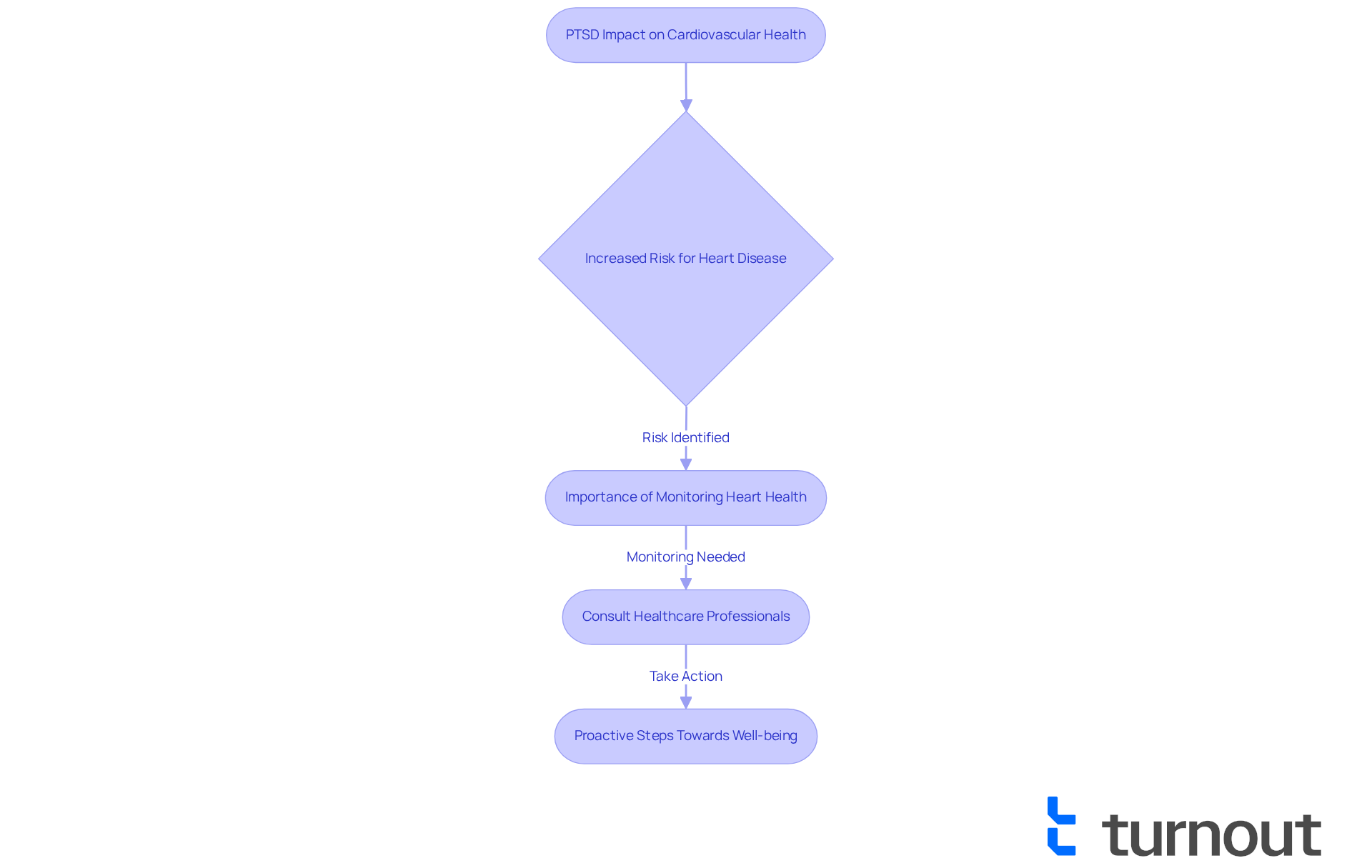
Cardiovascular Disease: A Serious Secondary Condition Associated with PTSD
Cardiovascular illness poses a significant risk for individuals suffering from PTSD secondary conditions. The tension and worry associated with PTSD can increase the likelihood of heart attacks and strokes. Research shows that individuals with PTSD secondary conditions face a higher risk for cardiovascular issues, with heart disease being notably more prevalent in this population. Dr. Roxana Mehran, a respected expert in cardiovascular research, emphasizes that emotional trauma can manifest physically, particularly affecting heart function.
It's crucial for former service members to prioritize their cardiovascular health. By consistently monitoring their heart conditions and consulting healthcare professionals for preventive strategies, they can take proactive steps toward well-being. Understanding how PTSD impacts heart health not only supports personal wellness but can also strengthen claims for disability benefits related to PTSD secondary conditions. This ensures that veterans receive the support they truly deserve.
We understand that navigating these challenges can be overwhelming. You're not alone in this journey, and there are resources available to help you. Prioritizing your heart health is a vital step toward a healthier future.
Conclusion
Understanding the various secondary conditions associated with post-traumatic stress disorder (PTSD) is crucial for former service members seeking the support and benefits they deserve. We recognize that the impact of PTSD extends beyond mental health, leading to a range of physical health issues such as migraines, sleep apnea, GERD, and more. Acknowledging these connections can empower veterans to advocate for their health and navigate the complexities of the benefits system.
Throughout this article, key insights highlight the importance of awareness and proactive management of these secondary conditions. It’s significant to note the prevalence of migraines and erectile dysfunction among veterans, alongside the serious implications of hypertension and cardiovascular disease. Clearly, PTSD can have far-reaching effects on overall well-being. Organizations like Turnout play a vital role in providing the necessary resources and support, ensuring that veterans are not alone in their journey toward recovery.
Ultimately, addressing PTSD and its secondary conditions is not just about managing symptoms; it is about reclaiming a quality of life that many veterans fought to protect. By prioritizing health, seeking appropriate care, and leveraging advocacy resources, former service members can navigate their challenges more effectively. We understand that the journey may be daunting, but with the right support, it is possible to overcome these obstacles and achieve a healthier, more fulfilling life.
Frequently Asked Questions
What is Turnout and what does it advocate for?
Turnout is dedicated to supporting former service members as they navigate the challenges of trauma and associated PTSD secondary conditions, ensuring they obtain the benefits and assistance they deserve.
What are PTSD secondary conditions?
PTSD secondary conditions are additional health issues that can arise from post-traumatic stress disorder, including diabetes, erectile dysfunction (ED), gastroesophageal reflux disease (GERD), and migraines.
How do PTSD secondary conditions affect veterans?
PTSD secondary conditions can complicate the benefits application process for veterans, making it harder for them to receive necessary assistance. They are also linked to a heightened risk of various health complications, including cardiovascular issues.
Why is understanding PTSD secondary conditions important for veterans seeking benefits?
Understanding PTSD secondary conditions is crucial because it can affect eligibility for benefits. Lack of awareness can lead to missed opportunities for support and resources.
How does Turnout assist veterans in navigating their benefits?
Turnout provides a streamlined approach to benefits navigation, utilizing technology like Jake, the AI case quarterback, to help service members manage applications, stay updated on deadlines, and receive proactive follow-ups.
What role do migraines play in the context of PTSD?
Migraines can be a significant issue for those with PTSD, as stress and anxiety can trigger episodes. Research shows a higher prevalence of migraines among veterans compared to the general population.
How can veterans access disability benefits for migraines?
To access disability benefits for migraines, veterans may need a nexus letter and supporting medical documentation, with the VA evaluating the severity based on the impact on daily life.
What is sleep apnea and how is it related to PTSD?
Sleep apnea is a condition that disrupts sleep patterns and can exacerbate fatigue and anxiety in veterans with PTSD. It is essential for veterans to recognize signs of sleep apnea and seek medical evaluation.
What are the treatment options for sleep apnea?
Treatment options for sleep apnea include Continuous Positive Airway Pressure (CPAP) therapy, lifestyle modifications, and Cognitive Behavioral Therapy for Insomnia (CBT-I).
Why is addressing sleep apnea important for veterans?
Addressing sleep apnea is crucial as it can improve overall health, enhance treatment effectiveness for PTSD, and potentially lower the risk of cardiovascular problems associated with untreated sleep apnea.




