Introduction
The alarming rise of sleep apnea among military personnel is a serious concern that affects not just individual health but also operational effectiveness. We understand that service members face unique stressors - ranging from unpredictable rest patterns to the physical and psychological toll of combat. This has led to a dramatic increase in the prevalence of obstructive sleep apnea.
It's crucial to recognize the intricate factors contributing to this condition. By understanding these elements, we can develop effective interventions that truly make a difference. How can the military better address the growing incidence of sleep apnea? This question is vital, as it touches on the well-being of our members and the readiness of our forces.
You are not alone in this journey. Together, we can explore solutions that support our service members and ensure they receive the care they need.
Defining Sleep Apnea: A Military Perspective
Obstructive breathing interruptions during rest can be a significant challenge, especially for our brave armed forces members. We understand that this condition occurs when throat muscles relax, blocking the airway. This can lead to serious health concerns, including daytime fatigue, impaired cognitive function, and an increased risk of accidents.
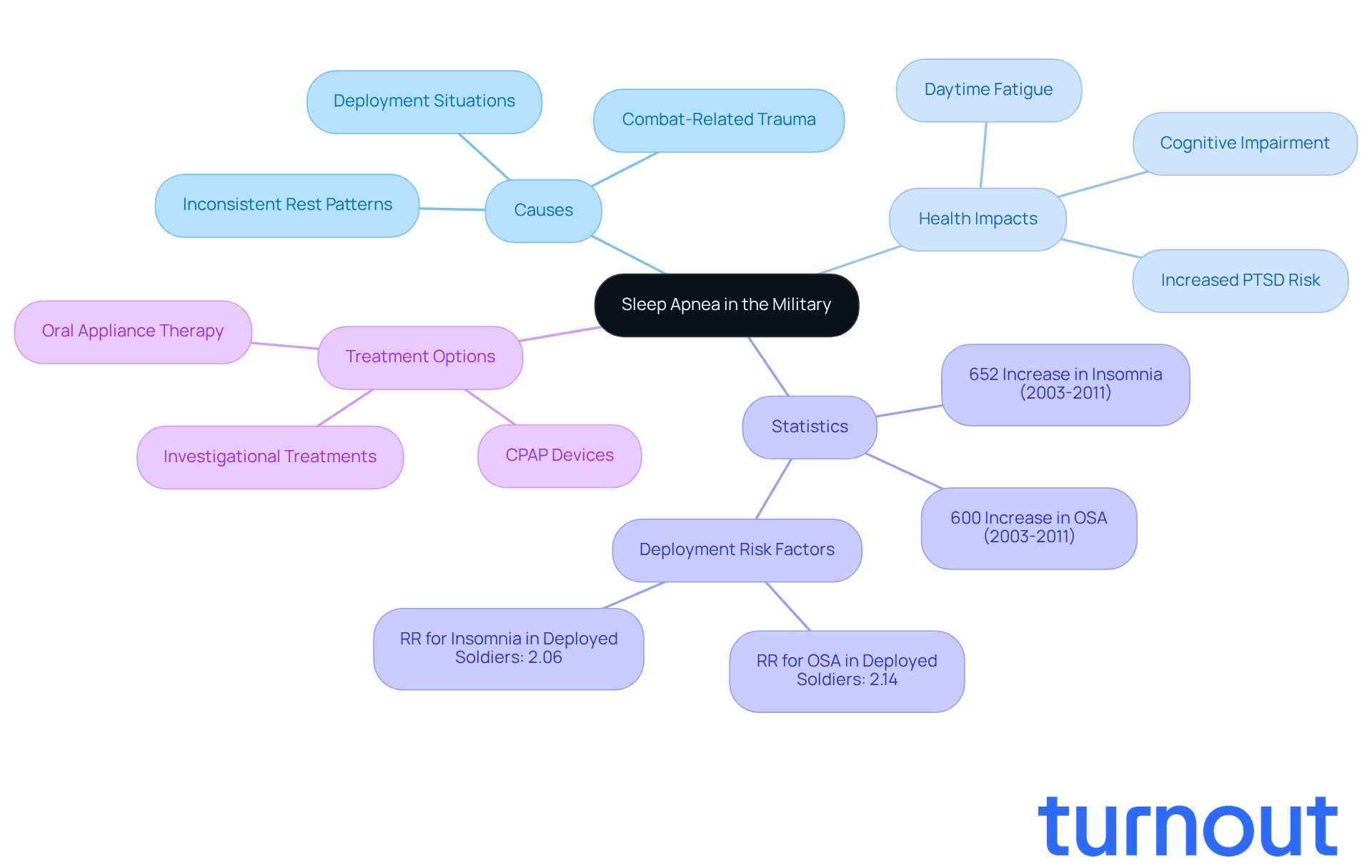
The lifestyle of armed forces personnel, marked by inconsistent rest patterns, deployment situations, and exposure to combat-related trauma, highlights what causes sleep apnea in the military and can worsen the risk and severity of disrupted breathing during sleep. Alarmingly, the increase in what causes sleep apnea in the military has resulted in a 600% surge in the incidence of obstructive sleep apnea (OSA) among U.S. Army soldiers from 2003 to 2011. This statistic highlights the urgent need for awareness and intervention.
The increased risk of being diagnosed with OSA among soldiers deployed for extended periods raises concerns about what causes sleep apnea in the military compared to their non-deployed counterparts. This concerning trend underscores the broader effects of sleep disorders on military readiness and overall well-being. Untreated sleep issues can lead to reduced efficiency and increased psychological health challenges, including PTSD and depression. In fact, soldiers with breathing disorders are over four times more likely to experience PTSD. This emphasizes the critical need for effective treatment options.
The armed forces are actively exploring various treatment devices for insomnia, which could pave the way for addressing this pressing concern. Understanding these dynamics is essential for meeting the health needs of our service members and ensuring their operational effectiveness. Remember, you are not alone in this journey, and we’re here to help.
Identifying Risk Factors for Sleep Apnea in Active-Duty Military
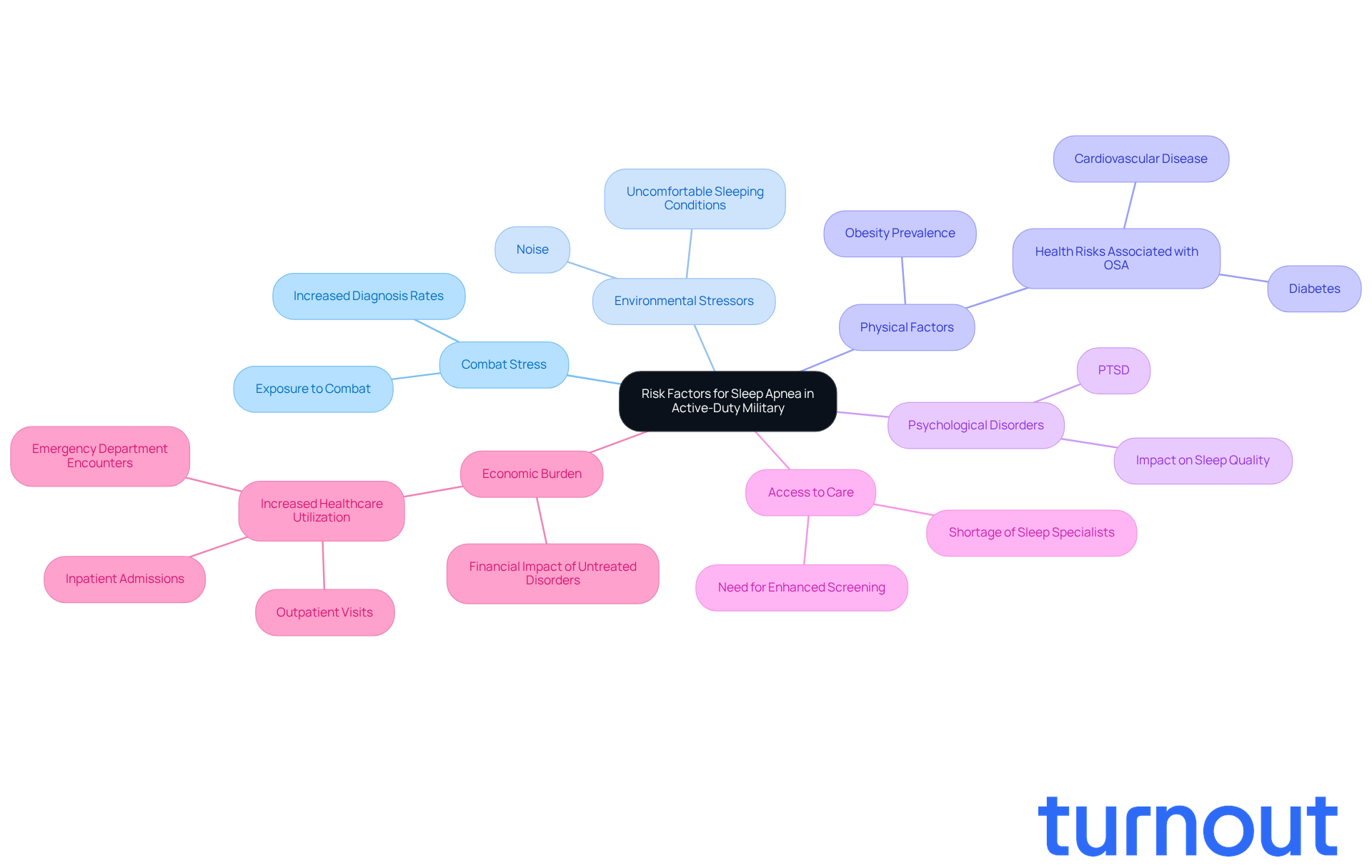
Active-duty military personnel face numerous challenges that can significantly impact their sleep health. We understand that exposure to combat stress is a major factor in what causes sleep apnea in the military, often resulting in higher rates of diagnoses among service members. Unpredictable rest patterns from deployments only add to this struggle, compounded by environmental stressors like noise and uncomfortable sleeping conditions.
Physical factors, particularly obesity - which is notably prevalent in armed forces populations - also play a critical role in sleep issues. Additionally, psychological disorders such as PTSD are common among veterans, further increasing the risk of disrupted rest. It's concerning to note that studies show what causes sleep apnea in the military, as servicemembers subjected to combat are almost three times more likely to receive a diagnosis of obstructive sleep apnea (OSA) within a year. This highlights the urgent need for focused interventions to address these unique challenges faced by our armed forces personnel.
Access to care is another pressing issue, with fewer than 40 active-duty physicians specializing in sleep medicine within the armed forces health system. This limitation can leave many without the support they need. The economic burden of untreated sleep disorders is significant as well. Servicemembers with OSA incur an additional 170,511 outpatient visits, 66 inpatient admissions, and 1,852 emergency department encounters annually.
This underscores the urgent requirement for enhanced screening and treatment protocols. It's important to recognize that the diagnosis of sleep disorders in the armed forces has risen dramatically, from 11 to 333 cases per 10,000 personnel between 2005 and 2019. We’re here to help, and together, we can work towards better solutions for those who serve our country.
Exploring the Impact of Sleep Apnea on Military Health and Operations
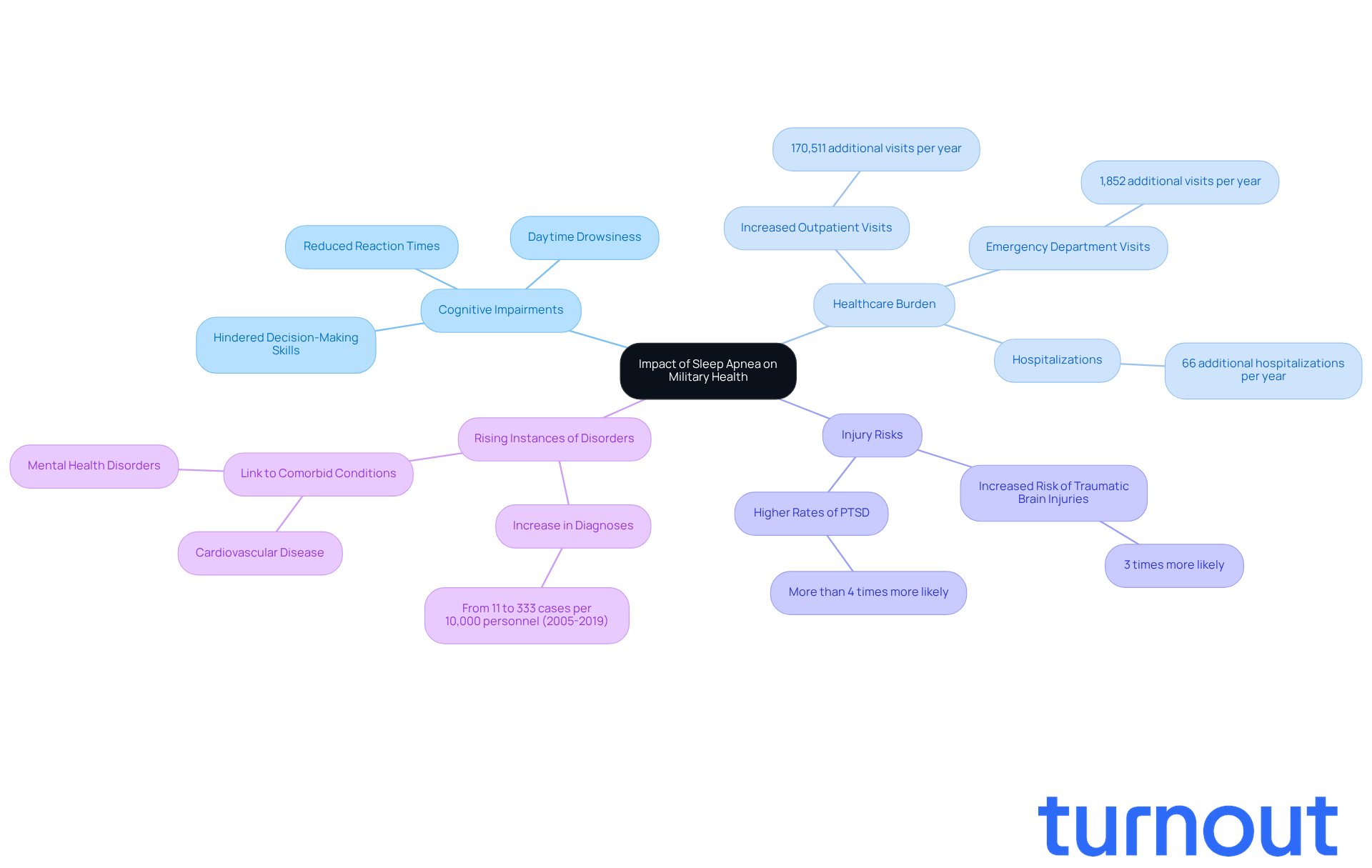
The significant impact of rest disruption on the health of our armed forces highlights what causes sleep apnea in the military, affecting both individual service members and the overall efficiency of defense operations. We understand that service members who experience disrupted rest often face considerable daytime drowsiness. This can greatly hinder cognitive functions, such as reaction times and decision-making skills. Such impairments not only increase the risk of accidents during critical missions but also lead to a higher occurrence of injuries among personnel. Studies reveal that military personnel with unaddressed rest disorders are three times more likely to sustain traumatic brain injuries and face elevated rates of post-traumatic stress disorder, complicating their medical profiles further.
Moreover, untreated nocturnal breathing issues, including what causes sleep apnea in the military, are linked to various comorbid conditions, such as cardiovascular disease and mental health disorders. These can negatively impact the preparedness and resilience of our military personnel. For instance, service members diagnosed with a sleeping disorder had an additional 170,511 outpatient visits and 1,852 emergency department visits in the year following their diagnosis. This highlights the significant healthcare burden associated with these conditions. As Col. Vincent Capaldi II poignantly stated, "This study is a wake-up call. Sleep disruption is not just a medical condition - it’s a force readiness issue." Addressing what causes sleep apnea in the military during rest is vital for sustaining a fit and efficient fighting force, as it directly relates to operational performance and the long-term health of our service members.
Furthermore, the identification of respiratory disorders in the armed forces has surged from 11 to 333 instances per 10,000 personnel between 2005 and 2019. This emphasizes the growing awareness of this crucial health concern. We’re here to help, and it’s essential to address these issues together. You are not alone in this journey.
Addressing Sleep Apnea: Solutions and Interventions for the Military
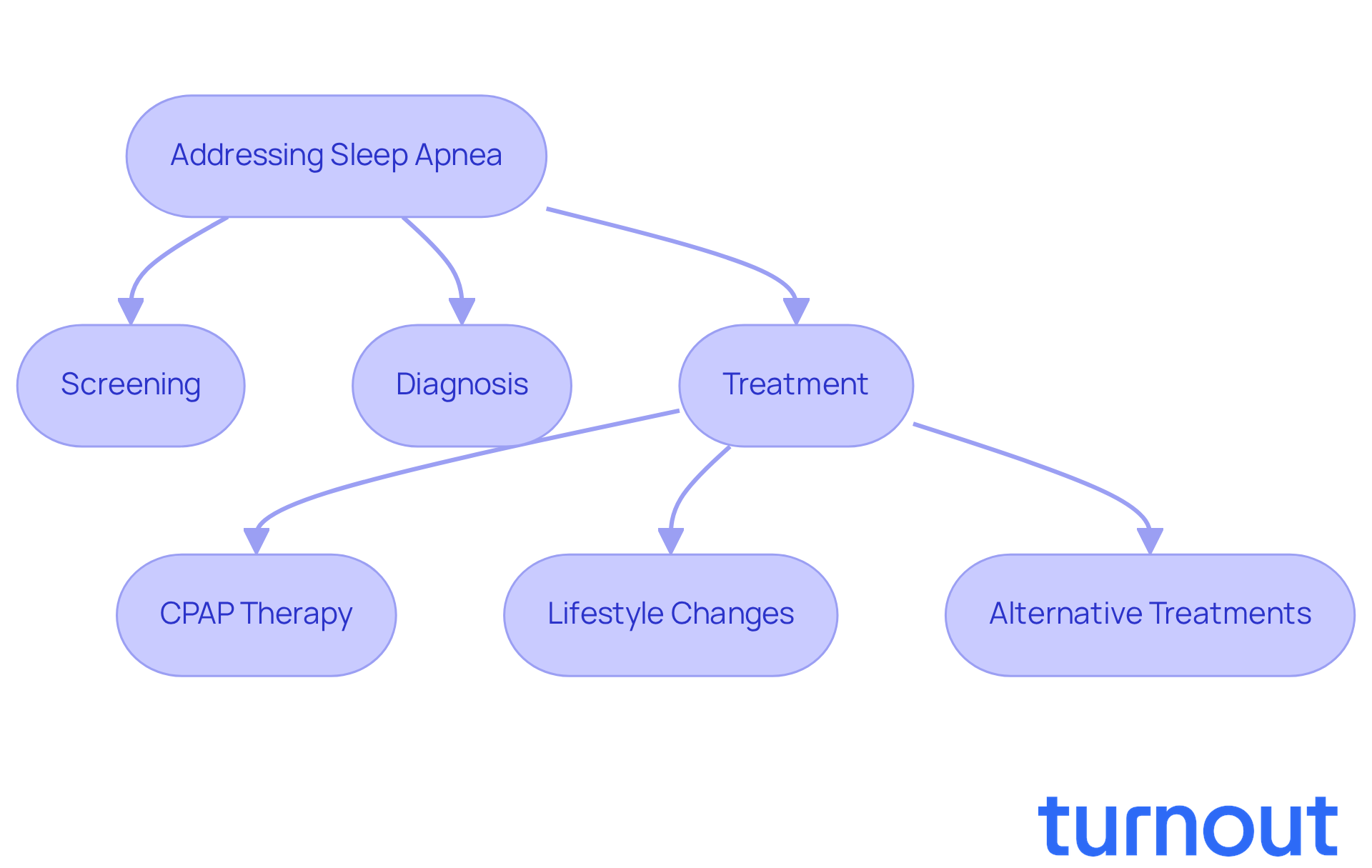
To effectively address what causes sleep apnea in the military, a comprehensive strategy that includes screening, diagnosis, and treatment is required. We understand that this can be a challenging journey. Continuous positive airway pressure (CPAP) therapy remains the gold standard, effectively keeping airways open during sleep. Alongside CPAP, lifestyle changes - like weight management, hygiene education related to rest, and stress reduction techniques - can significantly alleviate symptoms.
Recognizing the vital importance of sleep wellness, the military has launched various initiatives aimed at informing service members about sleep disorders, particularly focusing on what causes sleep apnea in the military, and improving access to necessary therapies. For instance, research shows that service members identified with a breathing disorder during sleep experience a significant increase in healthcare usage, with 170,511 extra outpatient appointments and 1,852 additional emergency department visits compared to their peers. This highlights the urgent need for effective management strategies.
Moreover, ongoing research into alternative treatments, including custom-made oral devices and surgical procedures, is essential for developing comprehensive care strategies for those affected by apnea. As Army Lt. Col. Christa Goodwin states, "Evidence shows that quality sleep contributes to enhanced physical and mental well-being, so addressing OSA can improve combat readiness." These initiatives reflect a growing acknowledgment within military circles regarding what causes sleep apnea in the military and emphasize that sleep health is integral to operational readiness and overall well-being.
You are not alone in this journey. We're here to help you navigate these challenges and find the support you need.
Conclusion
Understanding the causes of sleep apnea in military personnel is crucial for ensuring their health and operational readiness. This condition, marked by obstructed breathing during sleep, has become a significant concern within the armed forces. We recognize that factors like deployment stress, inconsistent sleep patterns, and physical health challenges - especially obesity - heighten the risk of sleep apnea among service members. The alarming rise in diagnoses calls for immediate attention and effective interventions.
The impact of sleep apnea on cognitive function and overall military performance cannot be overlooked. Service members grappling with this condition often experience increased daytime fatigue, which can compromise their decision-making abilities and operational effectiveness. It’s common to feel overwhelmed, especially when considering the correlation between sleep apnea and mental health disorders like PTSD. This emphasizes the importance of addressing the issue holistically. With limited access to specialized care, the need for improved screening and treatment protocols becomes even more pressing.
Ultimately, tackling sleep apnea in the military transcends medical concerns; it’s a matter of national security and the well-being of those who serve. Initiatives aimed at raising awareness, improving access to treatment, and fostering healthy sleep habits are essential for enhancing the quality of life for service members. We’re here to help ensure they are fit for duty. Prioritizing sleep health is imperative, as it not only benefits individual soldiers but also strengthens the overall effectiveness of the armed forces.
Frequently Asked Questions
What is sleep apnea and how does it affect military personnel?
Sleep apnea is a condition characterized by obstructive breathing interruptions during rest, occurring when throat muscles relax and block the airway. For military personnel, it can lead to serious health concerns such as daytime fatigue, impaired cognitive function, and an increased risk of accidents.
What factors contribute to sleep apnea in the military?
Factors contributing to sleep apnea in the military include inconsistent rest patterns, deployment situations, and exposure to combat-related trauma, which can worsen the risk and severity of disrupted breathing during sleep.
How has the incidence of obstructive sleep apnea (OSA) changed among U.S. Army soldiers?
There has been a 600% increase in the incidence of obstructive sleep apnea (OSA) among U.S. Army soldiers from 2003 to 2011, highlighting the urgent need for awareness and intervention.
How does deployment affect the diagnosis of sleep apnea among soldiers?
Soldiers deployed for extended periods are at a higher risk of being diagnosed with obstructive sleep apnea (OSA) compared to their non-deployed counterparts, raising concerns about the broader effects of sleep disorders on military readiness and well-being.
What are the psychological effects of untreated sleep apnea in military personnel?
Untreated sleep issues can lead to reduced efficiency and increased psychological health challenges, including PTSD and depression. Soldiers with breathing disorders are over four times more likely to experience PTSD.
What steps are being taken to address sleep apnea in the military?
The armed forces are actively exploring various treatment devices for insomnia and sleep apnea, aiming to meet the health needs of service members and ensure their operational effectiveness.




