Introduction
Sleep apnea is a serious concern for military personnel, with its prevalence alarmingly higher than in the general population. This raises important questions about the health and readiness of our brave armed forces members. We understand that the unique challenges faced by these individuals - ranging from deployment stressors to lifestyle factors - can create a complex web of causes behind this condition.
It's common to feel overwhelmed by the impact of sleep disturbances. These issues not only affect individual service members but also pose significant risks to operational effectiveness and overall military readiness. We’re here to help you navigate these challenges and find the support you need. Remember, you are not alone in this journey.
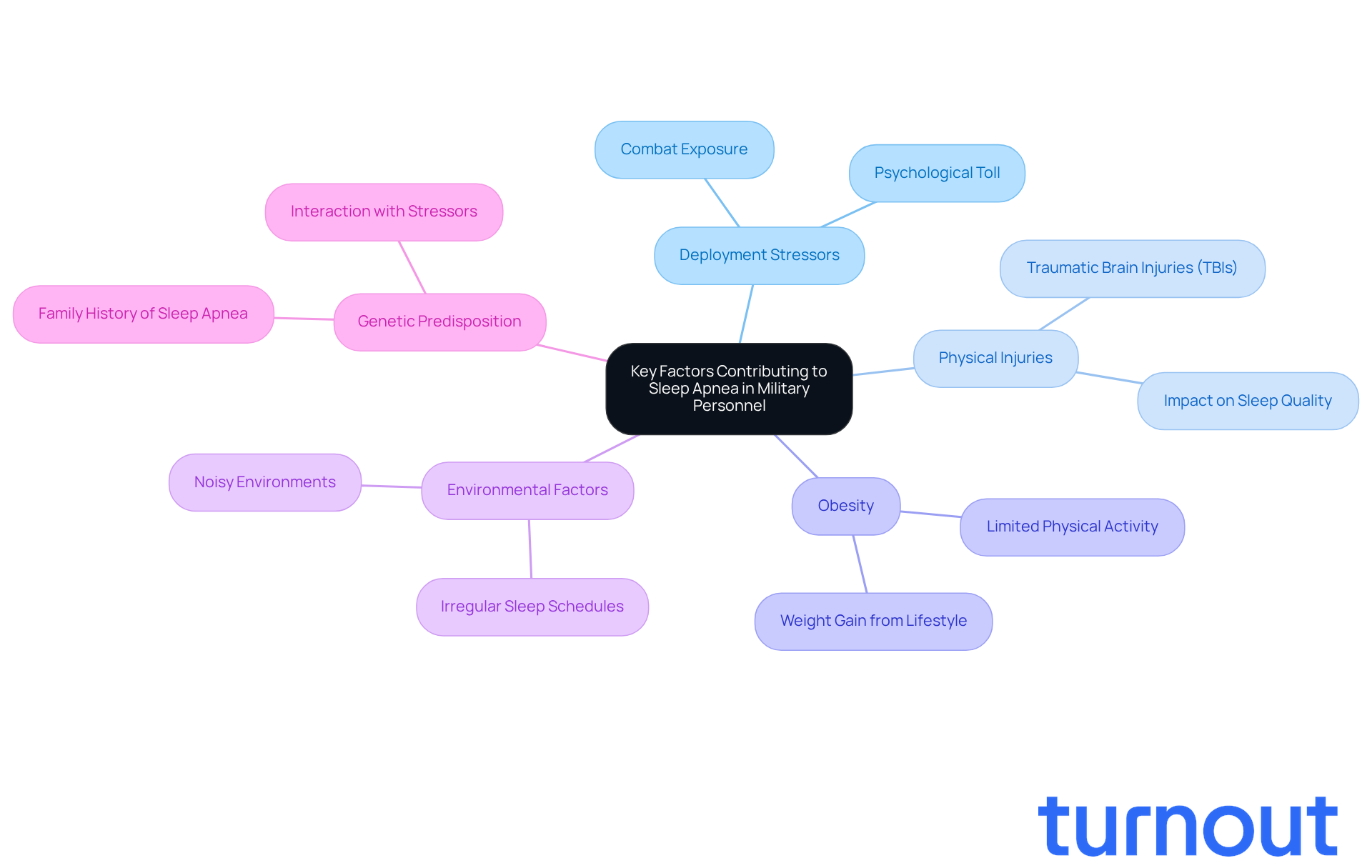
Identify Key Factors Contributing to Sleep Apnea in Military Personnel
Obstructive respiratory disturbance, particularly sleep apnea military, is notably more prevalent among armed forces members than in the general population. We understand that this disparity can be distressing, and several key factors contribute to it:
-
Deployment Stressors: Military personnel often face high-pressure situations during deployment, leading to disturbances in their rest. Research, including the case study "Combat Exposure and Deployment History Increase Insomnia, Sleep Disorders Risk," highlights that combat exposure and the psychological toll of military operations significantly contribute to sleep-related disorders.
-
Physical Injuries: Many service members sustain physical injuries that can affect their quality of rest. For instance, traumatic brain injuries (TBIs) are linked to increased occurrences of breathing interruptions at night, disrupting typical rest patterns.
-
Obesity: The lifestyle in the armed forces can lead to weight gain, a significant risk factor for disrupted breathing during sleep. Limited physical activity during certain deployments and dietary changes can exacerbate this issue.
-
Environmental Factors: Service members often rest in less-than-ideal conditions, such as noisy environments and irregular sleep schedules. These factors can disrupt slumber and increase the likelihood of developing sleep-related disorders.
-
Genetic Predisposition: Some individuals may have a genetic predisposition to sleep apnea, which can be worsened by the physical and psychological stresses of military life.
Understanding these elements is crucial for developing effective strategies and support systems for military members dealing with sleep apnea military and other breathing disorders during sleep. As Col. Vincent Capaldi noted, "This study is a wake-up call. Sleep disturbances are not just a medical condition - it’s a force readiness issue." Furthermore, as Emerson Wickwire emphasized, apnea during sleep is linked to various negative psychiatric and medical consequences, underscoring the importance of addressing this issue.
If you or someone you know is struggling with these challenges, remember: you are not alone in this journey. We're here to help.
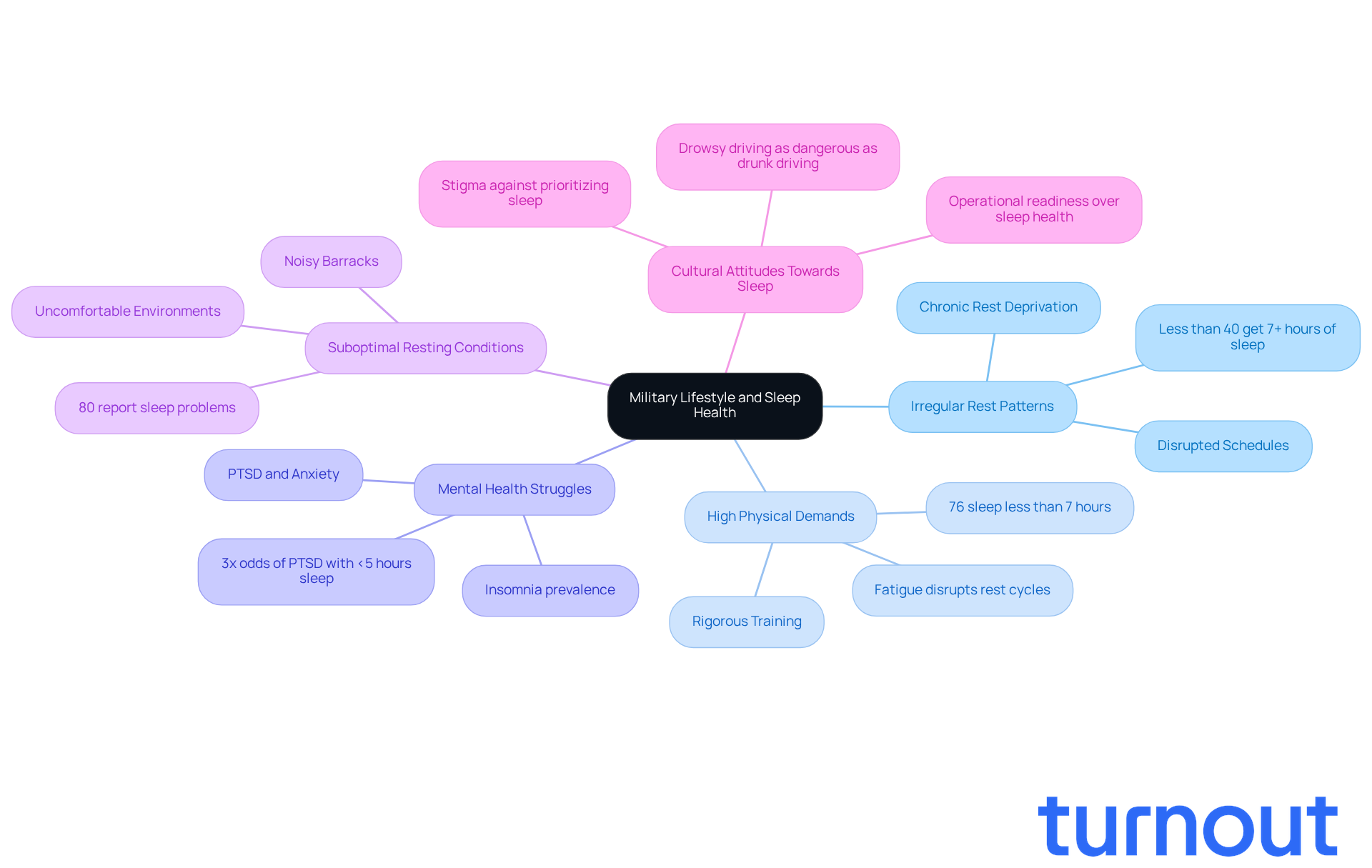
Examine Military Lifestyle and Its Effects on Sleep Health
The military lifestyle brings unique challenges that can deeply impact rest health. We understand that these challenges can feel overwhelming, but acknowledging them is the first step toward finding solutions. Here are some key factors to consider:
-
Irregular Rest Patterns: Military personnel often face disrupted rest schedules due to training exercises, deployments, and operational demands. This irregularity can lead to chronic rest deprivation, a significant risk factor for conditions like sleep apnea military. Research shows that fewer than 40% of nondeployed soldiers get more than seven hours of rest during the workweek, resulting in widespread rest-related issues.
-
High Physical Demands: The rigorous physical requirements of military training can lead to exhaustion, which paradoxically affects the quality of rest. Fatigue disrupts natural rest cycles, making it hard to achieve restorative slumber. Studies indicate that 76% of service members rest for fewer than the recommended seven hours each night, worsening fatigue-related problems.
-
Mental Health Struggles: Mental health disorders, including PTSD and anxiety, significantly impact rest quality among military personnel. These conditions often lead to insomnia and other disturbances, increasing the likelihood of developing sleep apnea military during sleep. A study found that veterans sleeping fewer than five hours a night had three times the odds of experiencing PTSD and major depressive disorder.
-
Suboptimal Resting Conditions: Service members frequently find themselves in environments that aren't conducive to restorative rest, such as noisy or uncomfortable barracks. This lack of a suitable resting environment can exacerbate rest issues, with 80% of post-9/11 veterans reporting sleep problems.
-
Cultural Attitudes Towards Sleep: Within the military, there's a cultural stigma that prioritizes operational readiness over sleep health. This mindset can diminish the focus on rest hygiene, contributing to the prevalence of sleep disorders. The Army acknowledges that drowsy driving is as dangerous as driving under the influence, yet operational demands often push soldiers to sacrifice rest.
By recognizing these lifestyle factors, we can better address the root causes of rest disturbances in our armed forces members. Together, we can promote necessary adjustments to enhance their rest health. Remember, you are not alone in this journey, and we're here to help.
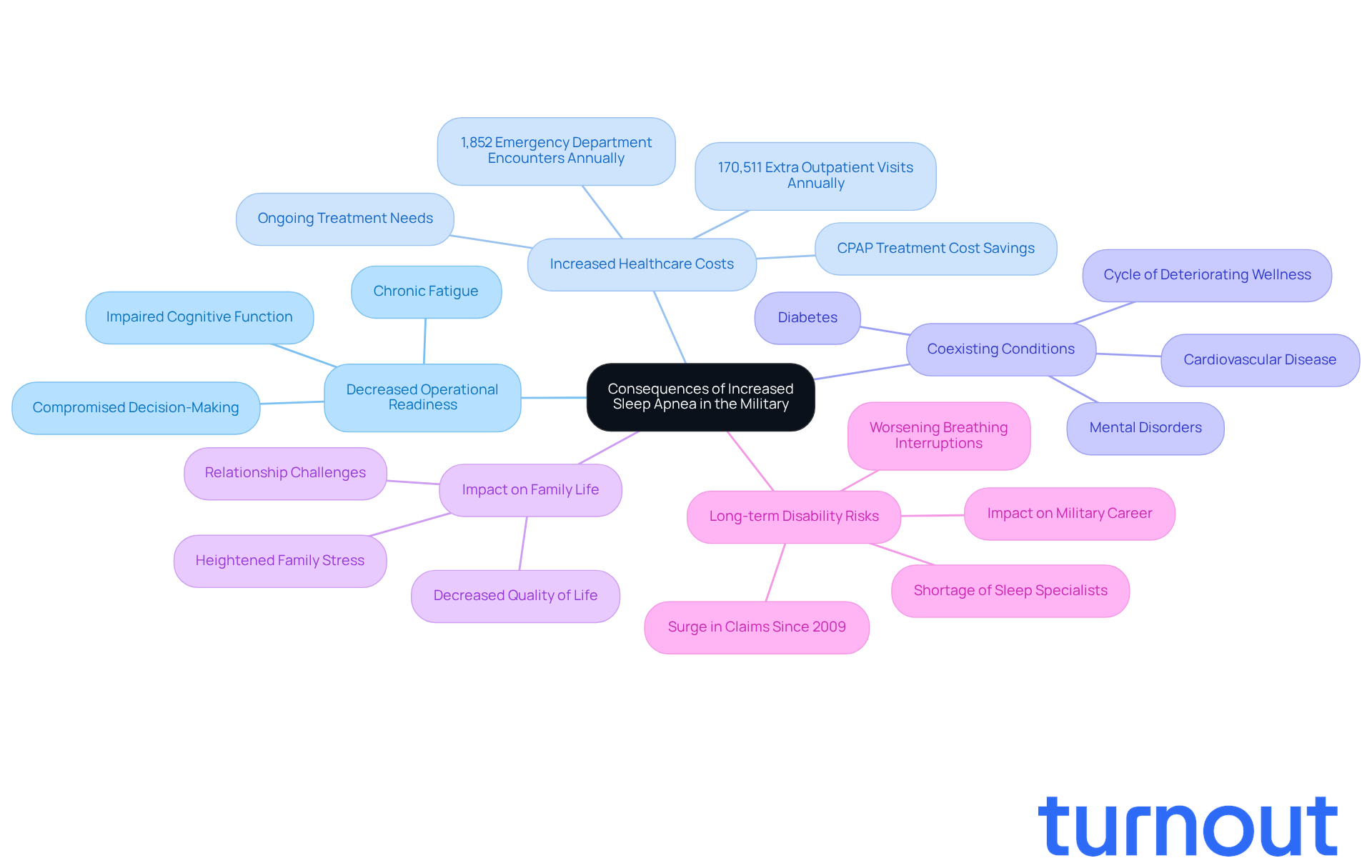
Analyze Consequences of Increased Sleep Apnea Rates in the Military
The rising rates of sleep apnea military personnel experience have significant consequences that we must address together.
-
Decreased Operational Readiness: We understand that sleep disorders can lead to chronic fatigue, which impairs cognitive function and decision-making abilities. This can compromise the operational readiness of armed units, as service members may struggle to perform effectively in high-stakes situations.
-
Increased Healthcare Costs: The financial burden related to a sleeping disorder is substantial. Service members diagnosed with sleep apnea military often require ongoing treatment, including CPAP therapy, which results in increased healthcare costs for both the military and the Department of Veterans Affairs. Research shows that service members with obstructive respiratory issues have 170,511 extra outpatient visits and 1,852 emergency department encounters each year. Furthermore, providing CPAP treatment for sleep apnea military can reduce the risk of dying from any cause by 37 percent, highlighting the potential cost-saving implications of effective treatment.
-
Increased rates of coexisting conditions highlight that untreated nocturnal breathing disturbances, such as sleep apnea military, can lead to feelings of being overwhelmed due to their association with various comorbidities, including cardiovascular disease, diabetes, and mental disorders. This can create a cycle of deteriorating wellness among service members, complicating their overall well-being and increasing healthcare utilization.
-
Impact on Family Life: The consequences of disrupted rest reach further than the individual service member. Families may experience heightened stress and strain due to the service member's health issues, potentially leading to relationship challenges and a decreased quality of life.
-
Long-term Disability Risks: As breathing interruptions during rest worsen, it can lead to long-term disability, impacting a service member's capacity to persist in their military career or shift to civilian life. This has enduring consequences for their financial stability and access to benefits. The substantial rise in claims for sleep apnea military disorders among veterans, which have surged more than elevenfold since 2009, underscores this issue. The shortage of qualified rest specialists within the Military Health System further complicates access to necessary care.
Addressing sleep apnea military is not just a wellness concern; it is vital for military preparedness and the overall welfare of service personnel and their families. Remember, you are not alone in this journey, and we're here to help.
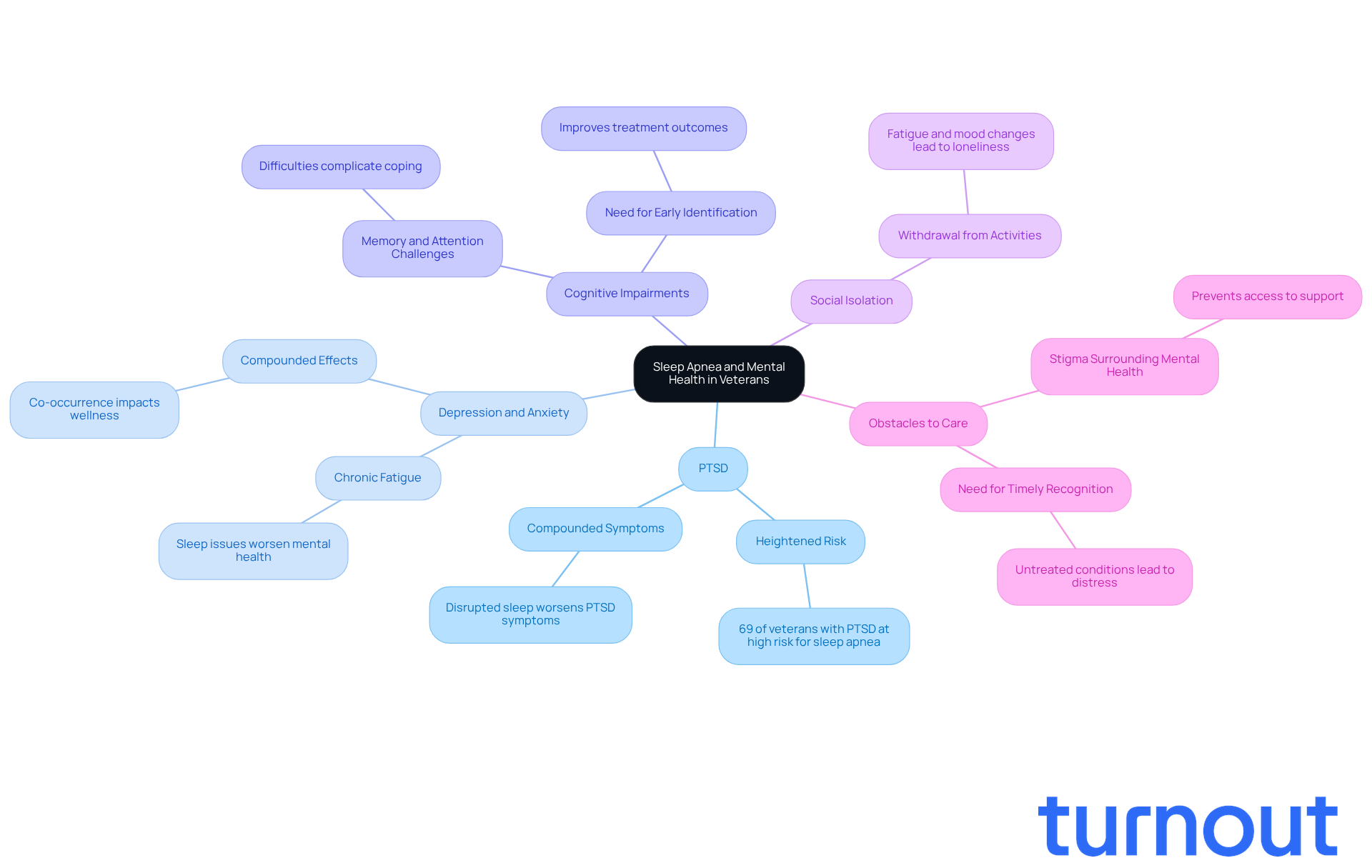
Connect Sleep Apnea with Mental Health Challenges in Veterans
The relationship between sleep apnea military and mental health challenges in veterans is complex and deeply intertwined. We understand that many veterans face significant struggles in this area, and it’s crucial to shed light on these connections:
-
Heightened Risk of PTSD: Research indicates that veterans who experience disrupted sleep are at a much higher risk of developing PTSD. The interruptions caused by breathing issues can intensify PTSD symptoms, creating a difficult cycle that feels overwhelming. In fact, a study revealed that 69% of veterans with PTSD also screened as high risk for sleep apnea military, highlighting this important link.
-
Depression and Anxiety: Sleep disturbances often accompany depression and anxiety disorders. The chronic fatigue and sleep issues tied to sleep disorders can either contribute to or worsen these mental health conditions, significantly impacting veterans' overall quality of life. The American Psychiatric Association emphasizes that when these conditions co-occur, they can have a compounded effect on wellness and well-being.
-
Cognitive Impairments: Sleep disruptions can lead to cognitive challenges, such as difficulties with memory, attention, and problem-solving. These cognitive hurdles can complicate psychological issues, making it harder for veterans to cope with their experiences and seek the help they need. Dr. Christopher J. Lettieri points out that early identification of sleep-disordered breathing can improve treatment outcomes for veterans with sleep apnea military.
-
Social Isolation: Veterans dealing with breathing difficulties during sleep may experience social isolation due to their health concerns. The fatigue and mood changes associated with disrupted sleep can lead to withdrawal from social activities, intensifying feelings of loneliness and depression.
-
Obstacles to Care: Many veterans encounter barriers when seeking treatment for sleep apnea, including stigma surrounding mental health issues. This stigma can prevent them from accessing the support they need, further complicating their health challenges. Ruchir Patel stresses that addressing these barriers is vital for improving the well-being and quality of life for veterans facing these issues. Timely recognition and action are essential, as untreated nighttime breathing disorders can lead to significant physical and emotional distress.
Recognizing the connection between sleep apnea military and mental health is essential for developing comprehensive treatment plans that address both physical and psychological health needs in veterans. Remember, you are not alone in this journey, and we’re here to help.
Conclusion
Understanding the complexities surrounding sleep apnea in military personnel is essential for addressing this pressing issue. We recognize the unique challenges faced by service members - deployment stressors, injuries, obesity, and environmental factors - that significantly contribute to the prevalence of sleep apnea. Acknowledging these influences is crucial for developing effective support systems that can help mitigate the impacts of this disorder on military readiness and the overall well-being of our service members.
The consequences of untreated sleep apnea are profound. They include decreased operational readiness, increased healthcare costs, and detrimental effects on mental health. It’s common to feel overwhelmed by the interconnection between sleep apnea and mental health challenges, such as PTSD and depression. This underscores the urgency of addressing both physical and psychological health needs in veterans. Furthermore, cultural attitudes within the military that prioritize operational readiness over sleep health only exacerbate these issues.
Ultimately, we must advocate for improved awareness and treatment options for sleep apnea among military personnel. By fostering an environment that prioritizes sleep health, the military can enhance operational effectiveness and support the overall quality of life for service members and their families. Addressing sleep apnea is not just a health concern; it’s a critical factor in maintaining the strength and readiness of our armed forces. Remember, you are not alone in this journey, and we’re here to help.
Frequently Asked Questions
What is sleep apnea and how does it relate to military personnel?
Sleep apnea is a disorder characterized by obstructive respiratory disturbances during sleep. It is notably more prevalent among military personnel than in the general population.
What are the key factors contributing to sleep apnea in military personnel?
The key factors include deployment stressors, physical injuries, obesity, environmental factors, and genetic predisposition.
How do deployment stressors affect sleep in military personnel?
Military personnel often experience high-pressure situations during deployment, which can lead to disturbances in their rest. Research indicates that combat exposure and the psychological toll of military operations significantly contribute to sleep-related disorders.
What role do physical injuries play in sleep apnea among service members?
Physical injuries, such as traumatic brain injuries (TBIs), can disrupt typical sleep patterns and are linked to increased occurrences of breathing interruptions at night.
How does obesity impact sleep apnea in military personnel?
A lifestyle that leads to weight gain, often due to limited physical activity and dietary changes during deployments, is a significant risk factor for disrupted breathing during sleep.
What environmental factors contribute to sleep disturbances in military personnel?
Service members often rest in noisy environments and have irregular sleep schedules, both of which can disrupt sleep and increase the likelihood of developing sleep-related disorders.
Is there a genetic component to sleep apnea in military personnel?
Yes, some individuals may have a genetic predisposition to sleep apnea, which can be exacerbated by the physical and psychological stresses of military life.
Why is addressing sleep apnea important for military readiness?
Sleep disturbances are considered a force readiness issue, as they can lead to various negative psychiatric and medical consequences, impacting the overall effectiveness of military personnel.




