Overview
Navigating long-term disability pregnancy benefits can be a daunting task for expectant mothers facing complications that might hinder their ability to work. We understand that this can be an overwhelming time, and having the right support is essential. This insurance provides crucial financial assistance during these challenging moments.
It's important to recognize the key strategies that can help you secure these benefits:
- Understanding eligibility criteria is vital.
- Maintaining thorough medical documentation is essential.
- Being proactive in the application process can make a significant difference.
Remember, complications can affect a considerable percentage of pregnancies, and you are not alone in this journey.
We encourage you to take these steps to ensure you receive the support you need. If you have any questions or concerns, please reach out. We're here to help you every step of the way.
Introduction
Navigating the complexities of long-term disability benefits during pregnancy can feel overwhelming for many expectant mothers. We understand that with complications affecting nearly 25% of pregnancies, grasping the nuances of this insurance is essential for ensuring financial security during such a vulnerable time. This guide aims to illuminate the eligibility criteria and application process, while also addressing the common challenges you may face when seeking these benefits.
What strategies can you employ to ensure you receive the support you need amidst the uncertainties of your health and employment? You're not alone in this journey, and we're here to help.
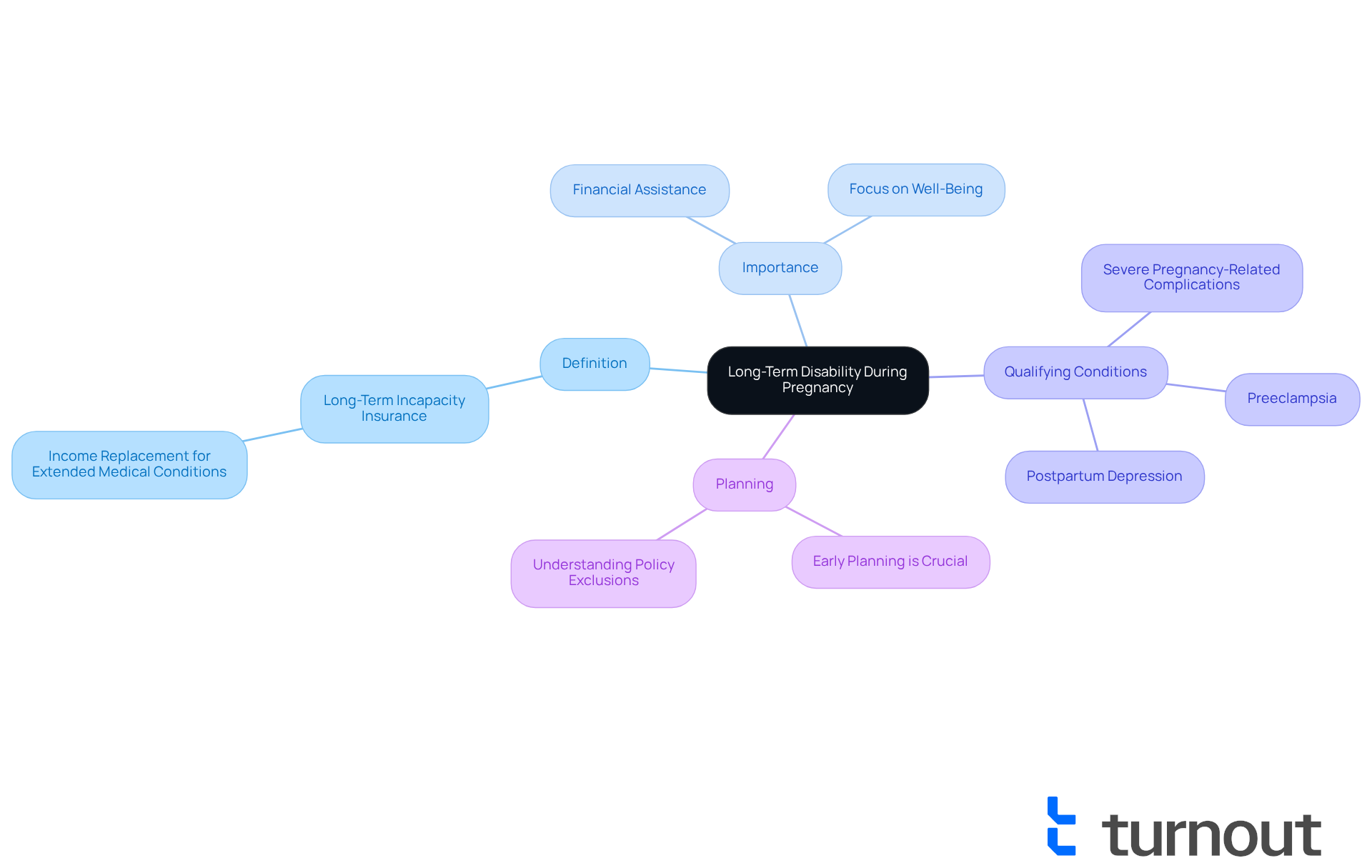
Define Long-Term Disability and Its Importance During Pregnancy
Long-term incapacity insurance is designed to provide income replacement for individuals unable to work due to a medical condition lasting for an extended period. This coverage becomes particularly vital during long-term disability pregnancy, as complications can arise that may impede a woman's ability to fulfill her job responsibilities.
We understand that navigating these long-term challenges can be overwhelming. This insurance offers financial assistance during a difficult time, allowing expectant mothers to focus on their well-being and that of their baby without the burden of financial stress. Conditions such as severe pregnancy-related complications, preeclampsia, and postpartum depression can qualify for long-term disability pregnancy benefits. In fact, complications affect up to 25% of pregnancies, underscoring the importance of being informed about your rights and options regarding long-term disability pregnancy coverage.
As Claudeth Henry wisely states, "Because complications from pregnancy are more frequent than many individuals understand," it is essential for women to secure suitable coverage for long-term disability pregnancy before conception. This ensures protection during this crucial period. Additionally, confirming insurance coverage for conditions related to long-term disability pregnancy prior to or soon after conception is essential. Understanding policy exclusions can help in preparing for potential claims.
Typically, there is a waiting period of 90 days or more before benefits are activated. Therefore, early planning is crucial. Remember, you are not alone in this journey; we’re here to help you navigate these important decisions.
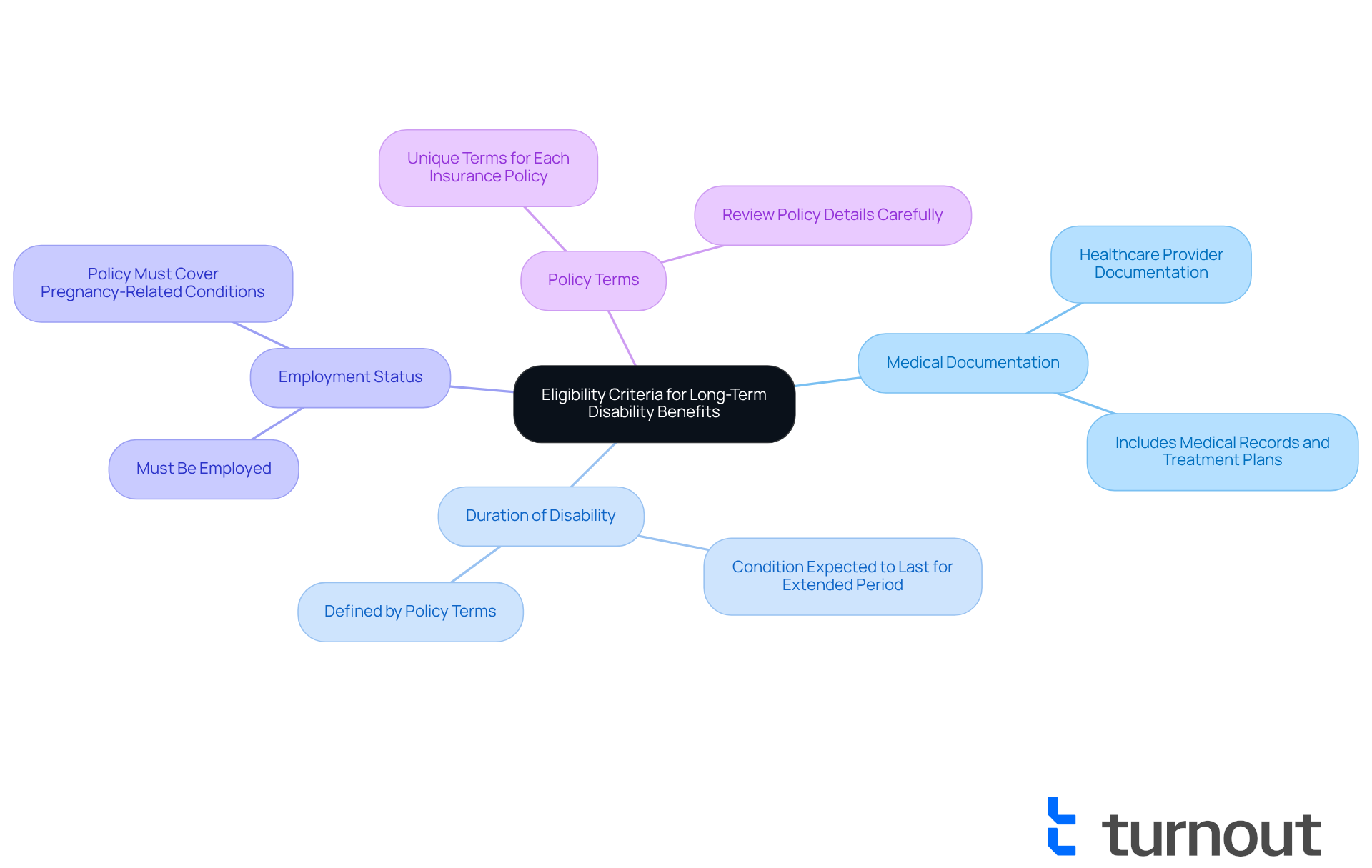
Outline Eligibility Criteria for Long-Term Disability Benefits During Pregnancy
To qualify for long-term disability pregnancy benefits, it’s essential to understand the criteria involved. We know this can be a challenging time, so let’s break it down together:
- Medical Documentation: A healthcare provider must document the pregnancy-related condition that affects your ability to work. This may include medical records, test results, and treatment plans.
- Duration of Disability: The condition should be expected to last for an extended period, often defined by your policy as exceeding a specific number of weeks.
- Employment Status: You must be employed and have a policy that covers pregnancy-related conditions.
- Policy Terms: Each insurance policy has unique terms regarding what qualifies as a condition, so reviewing your policy details carefully is crucial.
Understanding these criteria is vital for determining your eligibility and preparing for the application process related to long-term disability pregnancy.
When it comes to pregnancy-related health issues, comprehensive medical records play a significant role in successful requests. Did you know that nearly 22% of short-term benefits requests are due to pregnancies? This highlights the importance of having sufficient coverage. However, it’s concerning that over 51 million working adults in the U.S. lack adequate disability insurance beyond basic Social Security, which can lead to financial strain during unexpected health challenges.
Experts emphasize that thorough medical documentation is key to supporting your claims. This includes not only the diagnosis but also how the condition impacts your ability to perform your job. The reality is that the likelihood of missing work due to illness, injury, or long-term disability pregnancy is greater than many realize. By ensuring all necessary documentation is in place, you can significantly improve your chances of a successful request, especially given the critical need for comprehensive coverage.
Remember, you are not alone in this journey. We’re here to help you navigate these challenges and ensure you receive the support you deserve.
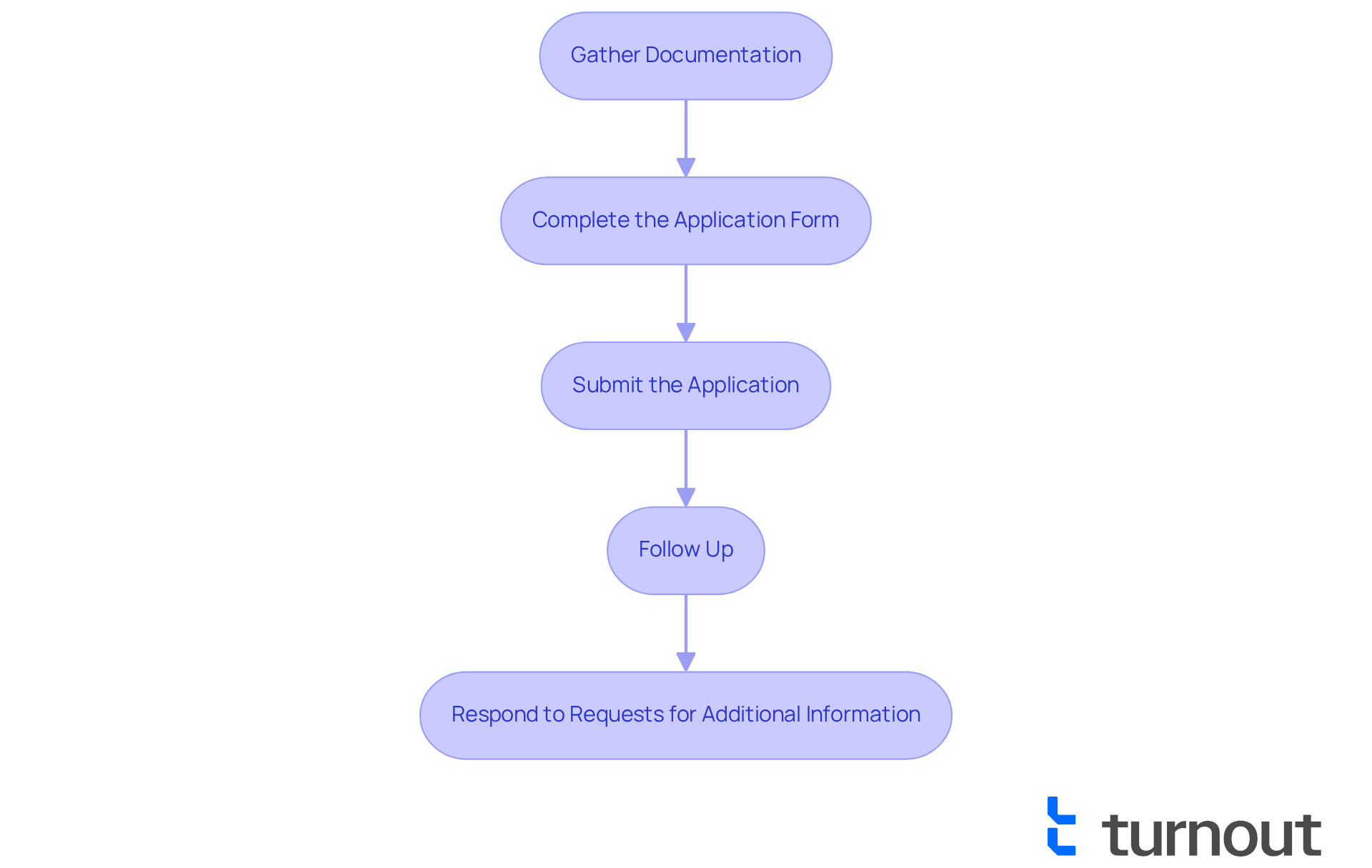
Detail the Application Process for Long-Term Disability Claims Related to Pregnancy
Navigating the application procedure for long-term disability pregnancy benefits can feel overwhelming. We understand that this journey is challenging, and we’re here to help you through it. The process generally includes several essential steps:
-
Gather Documentation: Start by collecting all necessary medical records. It's important to include detailed notes from your healthcare providers that outline your pregnancy-related condition. This documentation is crucial; insurers often require specific connections between your medical issues and job tasks. Dr. Sarah Chen emphasizes that general statements in medical records are frequently inadequate for claims. Comprehensive records are essential for successful applications.
-
Complete the Application Form: Take your time to accurately fill out the long-term impairment application form provided by your coverage provider. Ensure that all sections are thoroughly completed to avoid common mistakes that could lead to denials. Many individuals find themselves denied long-term disability pregnancy benefits on their first attempt, so attention to detail is vital.
-
Submit the Application: Once your application is complete, send it along with all supporting documents to your coverage provider. It’s wise to keep copies of everything you submit for your records.
-
Follow Up: After submission, check in with the provider to confirm receipt of your application and inquire about the processing timeline. It's common to feel anxious during this waiting period; maintaining ongoing communication is essential as insurers often continue investigating requests for compensation even after agreeing to pay them.
-
Respond to Requests for Additional Information: Be prepared to provide any further details or documentation the insurance company may request to support your application. This process can take time, so patience and persistence are key.
Statistics indicate that approximately 30 percent more women experienced both pregnancy and childbirth difficulties over the studied period. This underscores the importance of thorough documentation and persistence in claims. Additionally, be mindful of the waiting period that often begins on the day of incapacitation, during which no benefits are provided. Understanding these requirements and maintaining detailed records can greatly improve your chances of a successful application for long-term disability pregnancy. Remember, you are not alone in this journey.
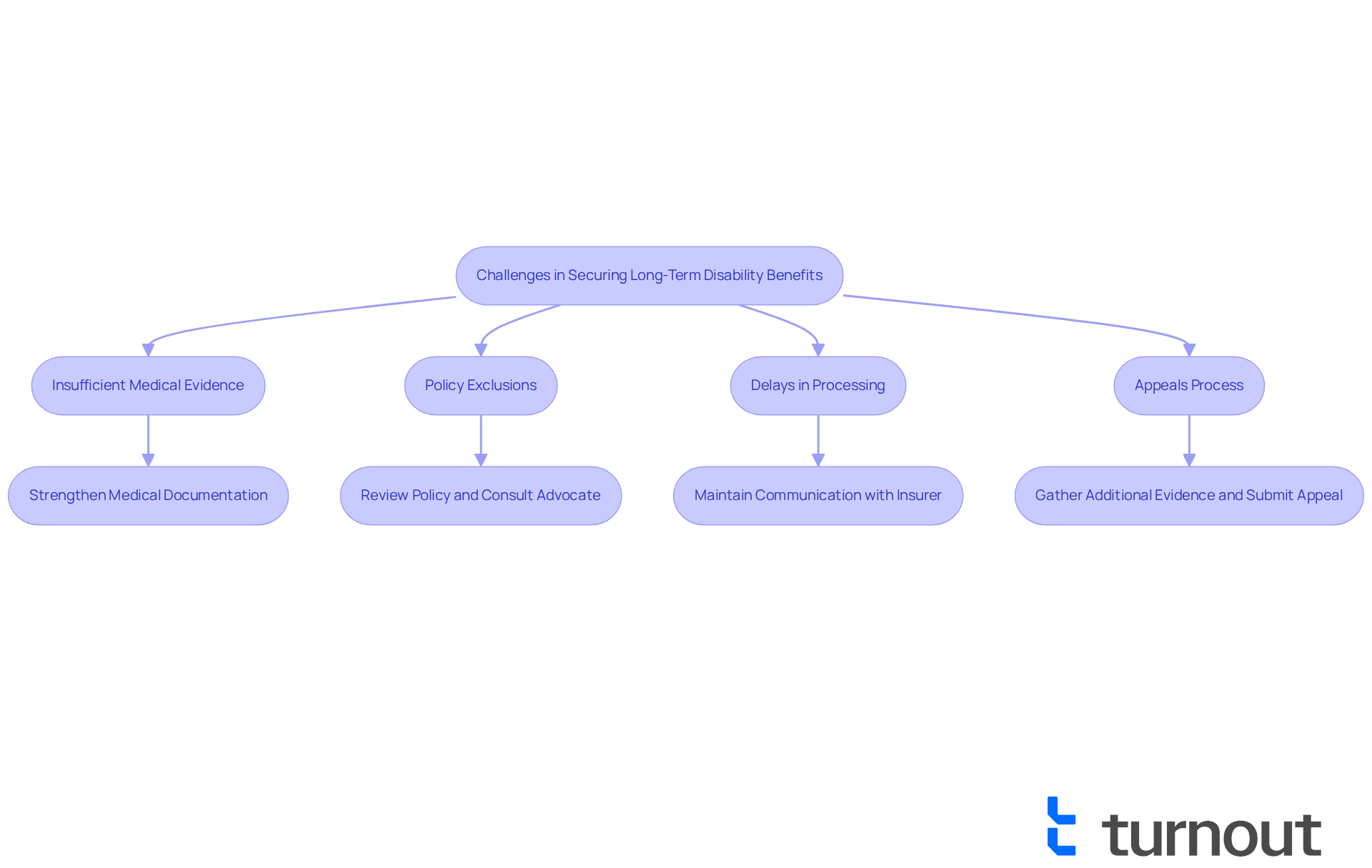
Identify Challenges in Securing Long-Term Disability Benefits and Strategies to Overcome Them
Securing long-term disability benefits can be a challenging journey, and we understand that you may feel overwhelmed. Here are some common obstacles you might face, along with supportive strategies to help you navigate them:
-
Insufficient Medical Evidence: Many claims are denied due to inadequate medical documentation. To strengthen your case, ensure that your medical records are thorough and clearly demonstrate how your condition impacts your ability to work. Keeping detailed notes from your healthcare providers can be invaluable in this process.
-
Some policies may have specific exclusions related to long-term disability pregnancy. It’s essential to review your policy carefully and consult with an advocate. Understanding your coverage and any limitations can empower you in your pursuit of benefits.
-
Delays in Processing: The reimbursement process can often be lengthy, leading to financial strain. To alleviate this stress, maintain open communication with your insurance provider and document all interactions. This proactive approach can help expedite processing times and keep you informed.
-
Appeals Process: If your claim is denied, knowing how to navigate the appeals process is crucial. Gather any additional evidence and submit a well-documented appeal that highlights new information supporting your case. Statistics show that those who prepare thoroughly and understand the appeals process have a significantly higher chance of success.
By being proactive and informed, you can navigate these challenges more effectively. Remember, you are not alone in this journey, and by turning potential obstacles into opportunities, you can secure the benefits you deserve.
Conclusion
Navigating long-term disability pregnancy benefits is a critical consideration for expectant mothers facing potential health challenges. We understand that securing appropriate coverage not only provides financial support during difficult times but also alleviates the stress associated with unexpected complications. Understanding the intricacies of long-term disability insurance is essential for ensuring that you are prepared and informed. This knowledge can significantly impact your well-being and that of your family.
Throughout this guide, we've highlighted key points, including:
- The importance of early planning
- The eligibility criteria for benefits
- The detailed application process
Emphasizing the need for comprehensive medical documentation and understanding policy exclusions can empower you to advocate for your rights effectively. It's common to face challenges in securing benefits, but employing strategic approaches to overcome them can enhance the likelihood of a successful claim.
Ultimately, the significance of long-term disability benefits during pregnancy cannot be overstated. By being proactive and informed, you can navigate this complex landscape with confidence. Take action now—review your insurance policies, gather necessary documentation, and seek support. Remember, you are not alone in this journey; we’re here to help ensure that your experience through pregnancy is as smooth and stress-free as possible.
Frequently Asked Questions
What is long-term disability insurance?
Long-term disability insurance is designed to provide income replacement for individuals who are unable to work due to a medical condition lasting for an extended period.
Why is long-term disability insurance important during pregnancy?
It is important during pregnancy because complications can arise that may impede a woman's ability to fulfill her job responsibilities. This insurance offers financial assistance, allowing expectant mothers to focus on their well-being and that of their baby without financial stress.
What types of complications can qualify for long-term disability pregnancy benefits?
Conditions such as severe pregnancy-related complications, preeclampsia, and postpartum depression can qualify for long-term disability pregnancy benefits.
How common are complications during pregnancy?
Complications affect up to 25% of pregnancies, highlighting the importance of being informed about rights and options regarding long-term disability pregnancy coverage.
When should women secure long-term disability coverage for pregnancy?
Women should secure suitable coverage for long-term disability pregnancy before conception to ensure protection during this crucial period.
What should women confirm regarding their insurance coverage related to long-term disability pregnancy?
It is essential to confirm insurance coverage for conditions related to long-term disability pregnancy prior to or soon after conception and to understand policy exclusions for preparing potential claims.
Is there a waiting period before long-term disability benefits are activated?
Yes, there is typically a waiting period of 90 days or more before benefits are activated, making early planning crucial.




