Introduction
Navigating the VA decision phase can feel overwhelming for veterans seeking disability benefits. This moment is crucial in determining eligibility, and it’s completely normal to feel anxious about it. Understanding the ins and outs of this process not only eases those worries but also empowers you to take meaningful steps toward a positive outcome.
We understand that the complexities involved can be daunting, and delays can add to the frustration. So, how can you ensure you’re ready to face this pivotal moment in your claims journey? By preparing yourself with the right information and support, you can tackle this challenge with confidence. Remember, you are not alone in this journey; we’re here to help.
Understand the VA Decision Phase
The VA decision phase represents a crucial step in your disability application process, during which the VA reviews your submitted documentation to determine your eligibility for benefits. We understand that this can be a challenging time, and knowing what to expect can help ease your concerns. Here’s what you need to know:
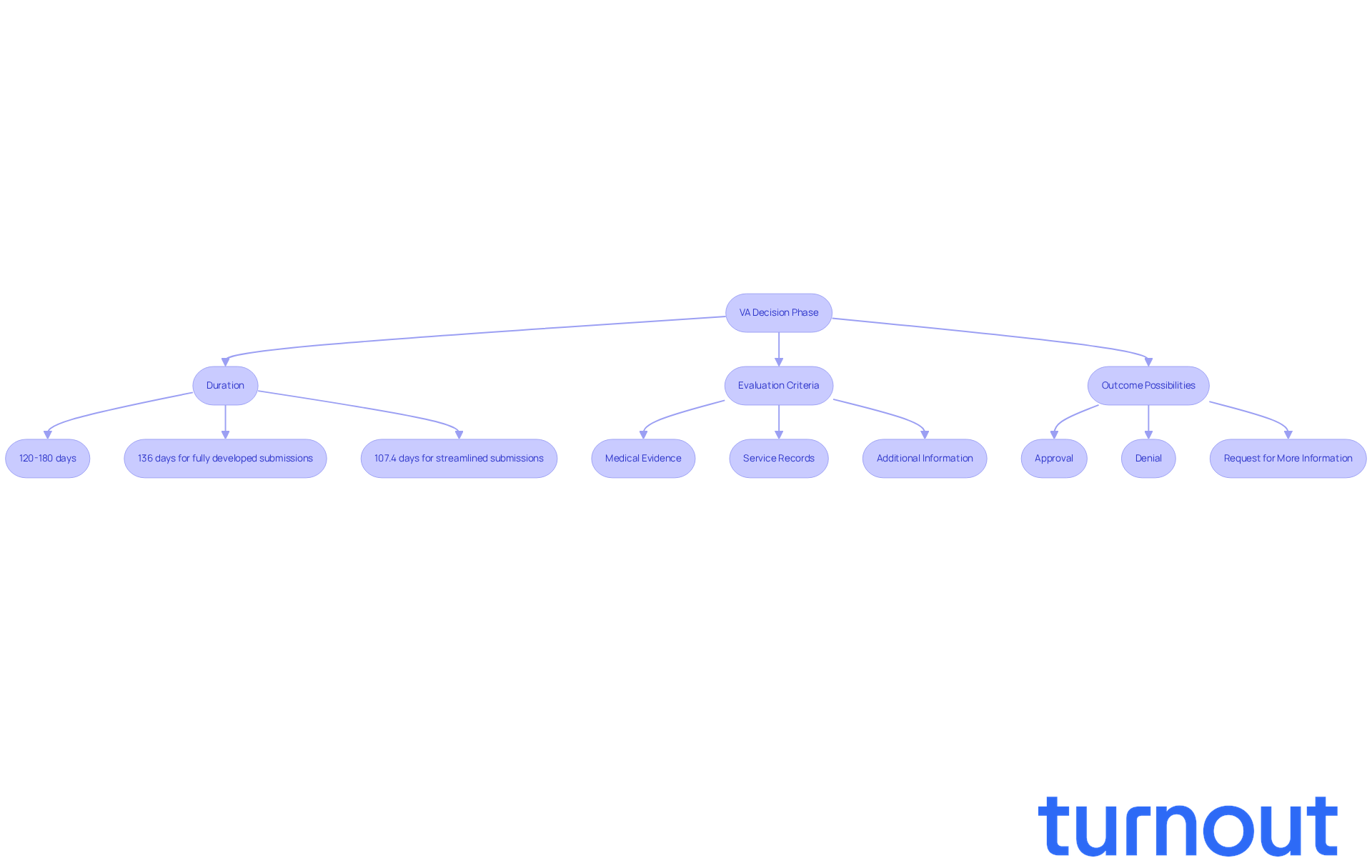
-
Duration: Typically, the VA takes between 120 to 180 days to reach a decision. This timeframe can vary based on the complexity of your request and the current volume of submissions. In 2025, fully developed submissions filed online are processed in about 136 days, while streamlined submissions average around 107.4 days.
-
Evaluation Criteria: The VA evaluates various factors, including medical evidence, service records, and any additional information you provide. For example, if you’ve been exposed to burn pits, your requests for conditions like chronic sinusitis may be expedited under new presumptive service connections. Understanding these criteria can significantly enhance your preparation and confidence.
-
Outcome Possibilities: The decision can lead to approval, denial, or a request for more information. Many veterans find that being proactive in responding to VA requests helps prevent unnecessary delays. One veteran shared, "I learned the hard way that responding quickly to any VA communication is crucial; it can make or break your claim timeline."
Recent changes in the VA evaluation process, including the expansion of digital systems for quicker retrieval of medical records and new community care contracts, aim to improve efficiency and access to benefits. By familiarizing yourself with these elements, you can navigate the VA decision phase with greater confidence and clarity. Remember, you’re not alone in this journey; we’re here to help.
Follow the Steps of the VA Decision Process
Navigating the VA decision process can feel overwhelming, but you’re not alone. Here are some essential steps to help you through:
-
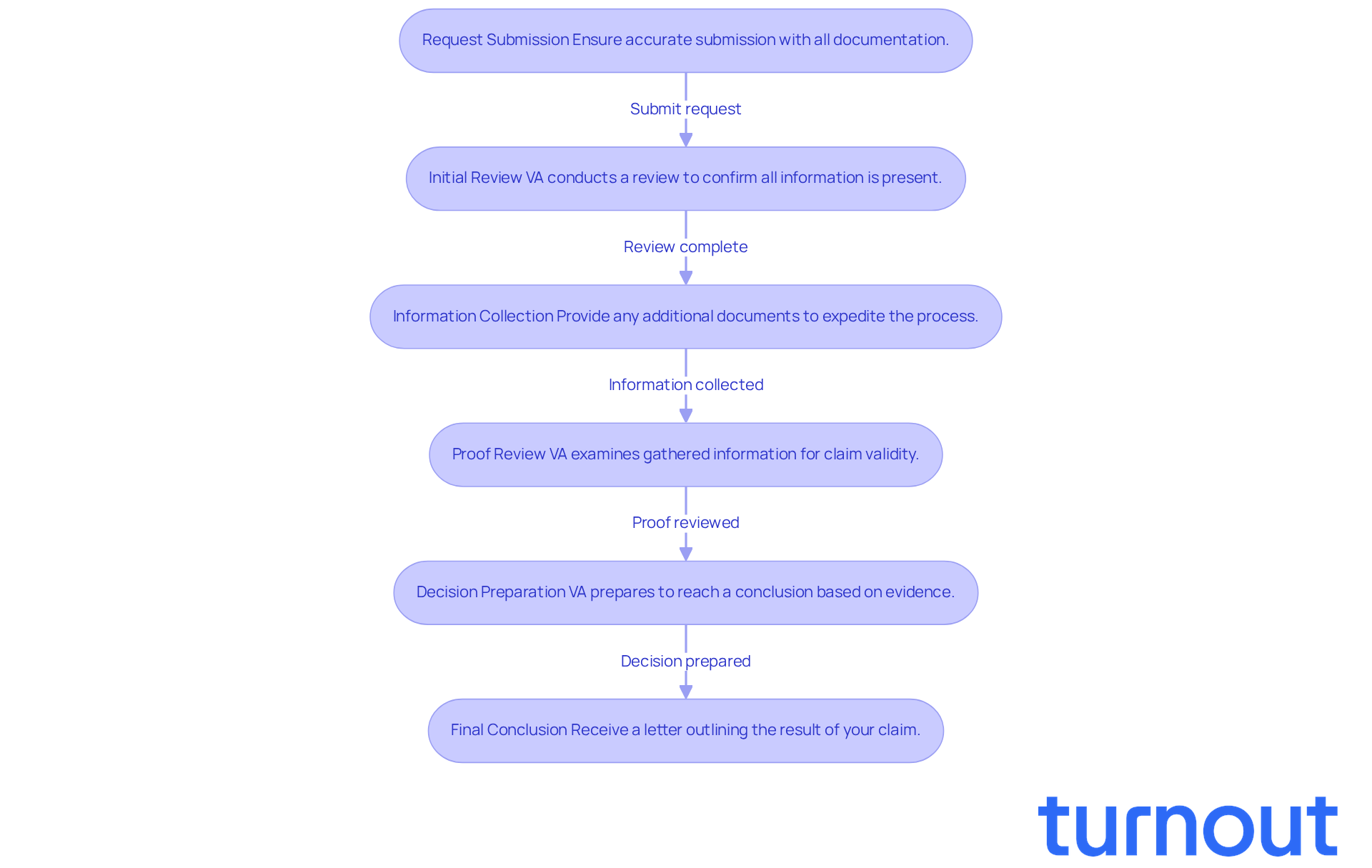
Request Submission: Start by ensuring your request is submitted accurately, including all necessary documentation. It’s crucial to check for completeness to avoid unnecessary delays. Remember, incomplete submissions can significantly extend processing times. As of September 2025, the VA has improved processing precision to 93.5%, underscoring the importance of precise submissions.
-
Initial Review: After you submit your request, the VA will conduct an initial review to confirm that all required information is present. This step typically takes a few weeks. It’s essential to ensure your request is fully developed to facilitate a smoother review. VA Secretary Doug Collins has said, "Veterans deserve prompt and precise decisions on their requests, and we anticipate continuing to provide outstanding outcomes to those who have worn the uniform."
-
Information Collection: Sometimes, the VA may need to collect additional information. Be proactive in providing any missing documents or information to expedite this process. Timely submissions can help avoid backlogs. With upcoming changes in 2025, especially regarding sleep apnea and tinnitus ratings, staying informed about how these updates may impact your case is vital.
-
Proof Review: Once all information is gathered, the VA will examine it to determine the validity of your claim. The quality and thoroughness of your submitted documents are crucial at this stage, as they directly influence the outcome.
-
Decision Preparation: The VA will prepare to reach a conclusion based on the reviewed evidence. This phase can take several weeks, so patience is key. Staying informed about your request's status can help you manage your expectations.
-
Final Conclusion: Finally, you will receive a letter outlining the result of your claim. This letter will explain the assigned rating and the rationale behind the decision, providing clarity on the next steps.
By following these steps, you can remain informed and engaged throughout the decision-making process. Remember, we’re here to help you enhance your chances of a favorable outcome.
Gather and Present Medical Evidence Effectively
Gathering and presenting medical evidence can feel overwhelming, but with the right approach, you can navigate this process successfully. Here are some caring guidelines to help you:
-
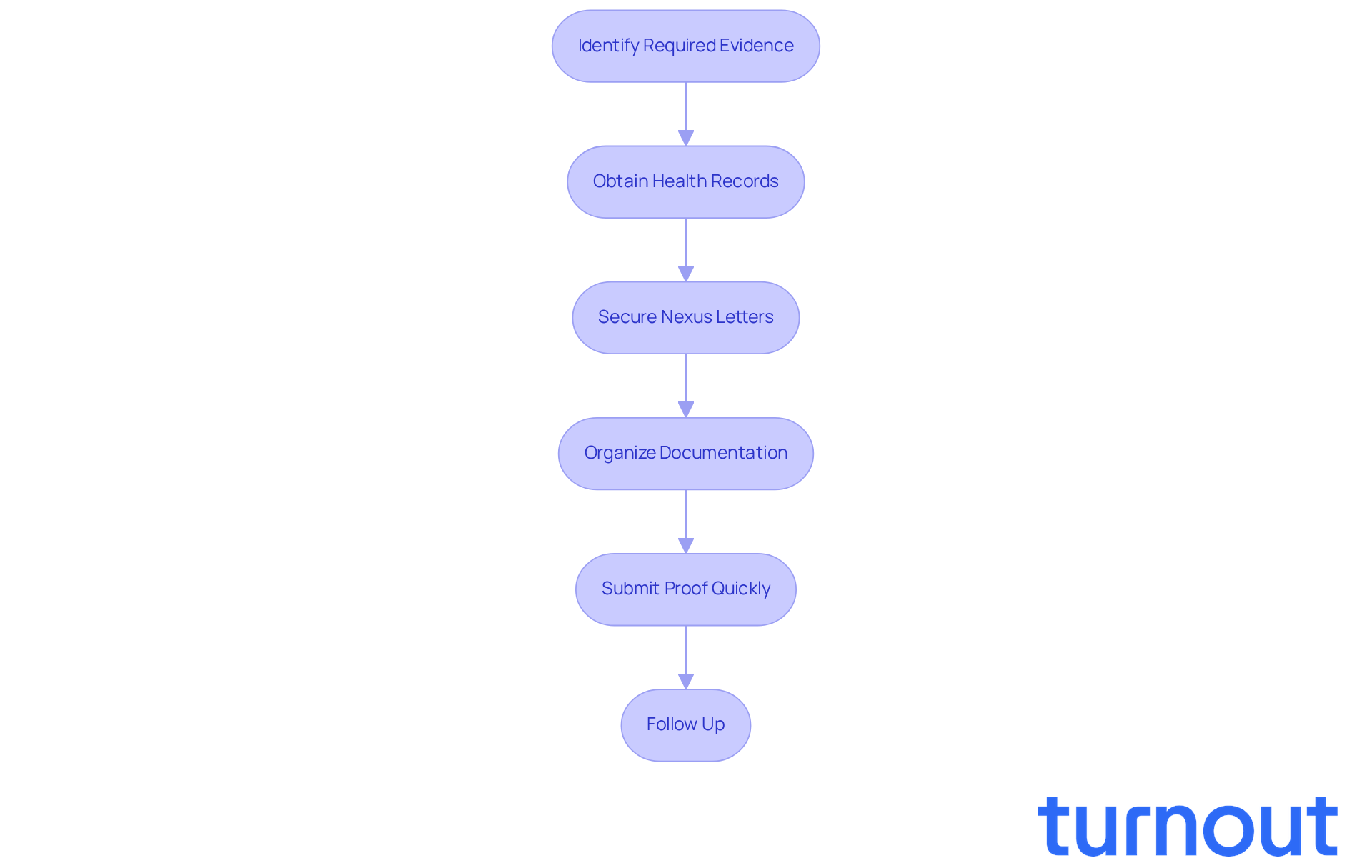
Identify Required Evidence: Start by determining the types of health evidence you need for your claim. This includes service treatment records, private health records, and relevant diagnostic tests. We understand that this can be a lot to manage, but taking it step by step will make it easier.
-
Obtain Health Records: Request copies of your health records from your healthcare providers. It’s important that these documents clearly outline your diagnosis and treatment history. Remember, you deserve to have all the information you need at your fingertips.
-
Secure Nexus Letters: Reach out to qualified health professionals for nexus letters that connect your service to your health condition. These letters are vital - they can significantly strengthen your claim by establishing that crucial link between your disability and military service. As Jordan Anderson, founder of VA Claims Academy, wisely points out, "A weak nexus letter with no rationale, no citation of medical literature, and no connection to the veteran’s actual service history is worthless."
-
Organize Documentation: Present your information clearly and in a structured manner. Using tabs or folders to organize different types of materials can help facilitate the VA decision phase. We know that clarity can make a big difference in how your case is perceived.
-
Submit Proof Quickly: Make sure to provide all your proof as soon as possible, ideally at the time of your submission. Delays can postpone the VA decision phase, making it essential to act swiftly. Did you know that over one-third of VA applications are rejected each year due to inadequate support? The average time to finalize disability-related requests is currently 81.1 days, so timely submissions are crucial.
-
Follow Up: After you submit your documentation, don’t hesitate to follow up with the VA. Confirm receipt and ask if any additional information is needed. This proactive step shows your commitment to your claim.
By efficiently collecting and showcasing your healthcare documentation, including strong nexus letters, you can bolster your requests and enhance your chances of a positive outcome. Remember, quality documentation is key; a weak nexus letter can undermine your claim. So, ensure your medical evidence is comprehensive and well-organized. You are not alone in this journey, and we’re here to help you every step of the way.
Explore Next Steps After the Decision
After receiving your VA decision, it’s important to know the next steps you can take:
-
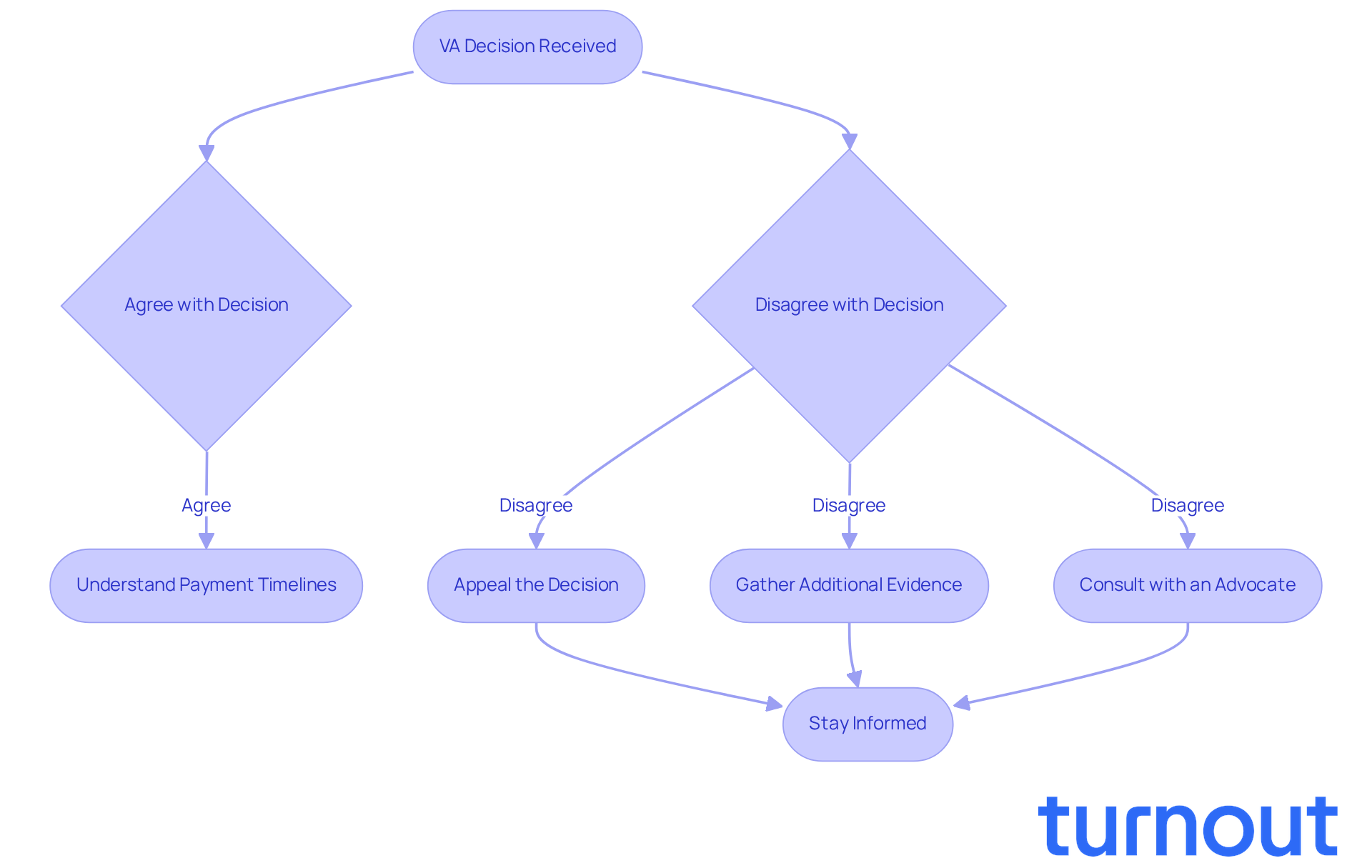
Review the Outcome Letter: Take a moment to carefully read the outcome letter. Understanding the result and the reasoning behind it is crucial. Pay close attention to your assigned disability rating and any conditions that may have been denied.
-
Accepting the Conclusion: If you agree with the conclusion, you might not need to take any further action. Just make sure you understand the payment timelines and how to access your benefits.
-
Appealing the Decision: If you disagree with the decision, remember that you have the right to appeal. Familiarize yourself with the different appeal options available, such as a Higher-Level Review or a Supplemental Claim. It’s common to feel uncertain about this process, but you’re not alone.
-
Gather Additional Evidence: Should you choose to appeal, consider gathering additional evidence to support your case. This could include new medical records or expert opinions that weren’t submitted before. Every bit of information can help strengthen your position.
-
Consult with an Advocate: If you’re feeling overwhelmed, reaching out to a disability benefits advocate can be a great step. Organizations like Turnout offer trained nonlawyer advocates who can guide you through the appeals process. They’re here to help you navigate these complex situations effectively, though it’s important to note that they do not provide legal advice.
-
Stay Informed: Keep track of your appeal status and any associated deadlines. Regularly checking in with the VA can ensure your appeal is progressing as it should.
By exploring these next steps, you can confidently and clearly navigate the aftermath of the VA decision phase. Remember, support is available through organizations like Turnout, and you don’t have to face this journey alone.
Conclusion
Navigating the VA decision phase is a crucial step for veterans seeking disability benefits. We understand that this process can feel overwhelming, but grasping its intricacies can truly influence the outcome of your claims. This phase involves a careful evaluation of the documentation you submit, which is essential in determining your eligibility for benefits. By preparing effectively and knowing what to expect, you can approach this journey with greater confidence and clarity.
In this article, we’ve outlined key steps to help you manage the VA decision phase successfully. From ensuring that your documentation is accurate to understanding the evaluation criteria, each detail plays a part in creating a smoother experience. Gathering comprehensive medical evidence, including nexus letters and well-organized documentation, is vital. And remember, knowing what to do after receiving a decision empowers you to take action-whether that means accepting the outcome or pursuing an appeal.
Ultimately, you don’t have to navigate the VA decision phase alone. With the right information, support, and proactive engagement, this process can lead to positive outcomes. We encourage you to stay informed, utilize available resources, and take charge of your claims to maximize your chances of success. The path may be challenging, but with determination and the right strategies, achieving the benefits you deserve is within reach. You're not alone in this journey; we're here to help.
Frequently Asked Questions
What is the VA decision phase?
The VA decision phase is a critical step in the disability application process where the VA reviews submitted documentation to determine eligibility for benefits.
How long does the VA typically take to reach a decision?
The VA usually takes between 120 to 180 days to reach a decision, but this timeframe can vary based on the complexity of the request and the volume of submissions.
What are the average processing times for fully developed and streamlined submissions?
In 2025, fully developed submissions filed online are processed in about 136 days, while streamlined submissions average around 107.4 days.
What factors does the VA evaluate during the decision phase?
The VA evaluates various factors, including medical evidence, service records, and any additional information provided by the applicant.
Are there expedited processes for certain conditions?
Yes, conditions related to exposures, such as burn pits, may be expedited under new presumptive service connections.
What are the possible outcomes of the VA decision?
The possible outcomes include approval, denial, or a request for more information from the applicant.
How can veterans prevent delays in their claims?
Many veterans find that being proactive in responding to VA requests can help prevent unnecessary delays in their claims.
What recent changes have been made to the VA evaluation process?
Recent changes include the expansion of digital systems for quicker retrieval of medical records and new community care contracts to improve efficiency and access to benefits.




