Introduction
Obsessive-Compulsive Disorder (OCD) is a mental health condition that affects millions of people. We understand that living with OCD can be incredibly challenging, often disrupting daily activities and relationships. This raises an important question: does OCD qualify for legal protections under the Americans with Disabilities Act (ADA)?
Exploring this topic is crucial, as it sheds light on the rights of individuals living with OCD. Recognizing OCD as a disability could transform the support available to those affected. It also prompts us to reflect on societal perceptions and the accommodations necessary for success in both personal and professional realms.
How can acknowledging OCD as a disability change the way we support individuals in their journey? You are not alone in this struggle, and together, we can advocate for the understanding and accommodations that can make a real difference.
Defining Obsessive-Compulsive Disorder (OCD)
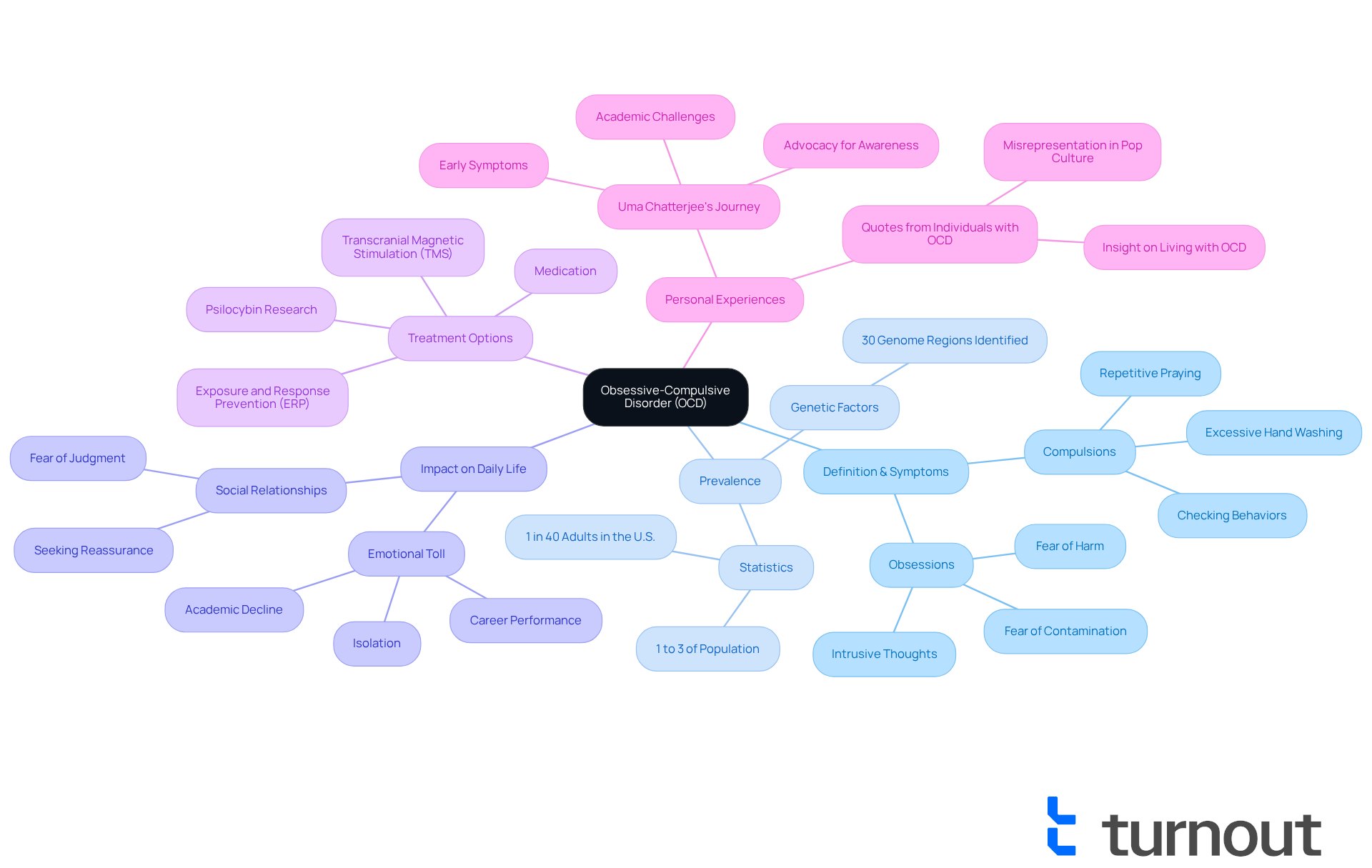
Obsessive-Compulsive Disorder (OCD) is a long-lasting psychological condition that many people struggle with. It’s characterized by persistent, unwanted thoughts-known as obsessions-and repetitive actions, or compulsions, that individuals feel compelled to perform. These obsessions can lead to significant anxiety, while the compulsions are often an attempt to alleviate that anxiety or prevent a feared event. For instance, someone with OCD might constantly worry about contamination, prompting them to wash their hands excessively.
We understand that OCD affects approximately 1% to 3% of the population, translating to about 1 in 40 adults in the U.S. This prevalent mental health disorder raises the question of whether OCD is considered a disability that can severely impact daily functioning. The emotional toll of untreated OCD is profound, leading many to ask if OCD is considered a disability, as it’s often regarded as one of the most debilitating conditions, resulting in isolation and hindering academic and career performance.
But there is hope. Effective treatments, such as exposure and response prevention (ERP) therapy, have shown considerable potential in helping individuals manage their symptoms. Mental health professionals note, "In ideal circumstances, ERP usually works better than medication." This highlights the importance of seeking the right support.
The experiences of individuals like Uma Chatterjee remind us of the urgent need for awareness and effective treatment options. Her journey illustrates the deep impact OCD can have on personal and social aspects of life. Remember, you are not alone in this journey. We’re here to help you find the support you need.
OCD as a Disability: Legal and Social Context
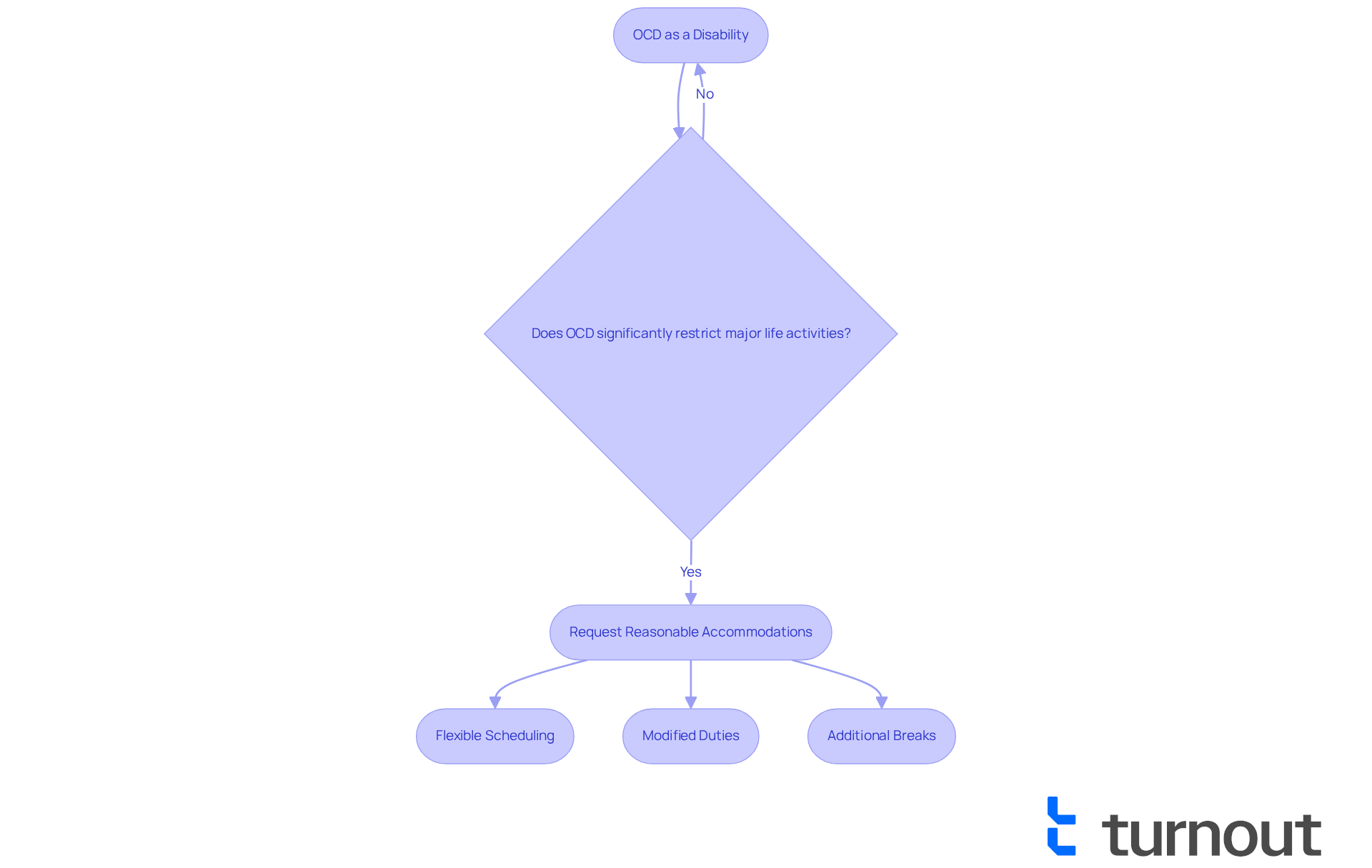
Under the Americans with Disabilities Act (ADA), is OCD considered a disability when it significantly restricts major life activities, such as work, learning, and social interactions? We understand that living with OCD can be challenging, and this raises the question of whether OCD is considered a disability, allowing individuals to request reasonable accommodations in the workplace. These accommodations might include:
- Flexible scheduling
- Modified duties
- Additional breaks to help manage symptoms effectively
For instance, if an employee struggles with timekeeping due to OCD, employers are obligated to consider adjustments that can facilitate better performance. Research shows that around 60% of people with OCD request reasonable accommodations at work. This highlights the importance of recognizing and addressing their needs, especially in the context of whether OCD is considered a disability. However, it’s common to feel hesitant about revealing one’s condition due to stigma and misconceptions surrounding OCD. This can complicate the ability to thrive in both personal and professional environments.
Advocates emphasize that promoting an inclusive workplace culture is crucial. By doing so, we can help those with OCD manage their challenges and obtain the accommodations they are entitled to under the law. Remember, you are not alone in this journey, and there are resources available to support you.
Key Characteristics of OCD and Their Impact on Daily Life
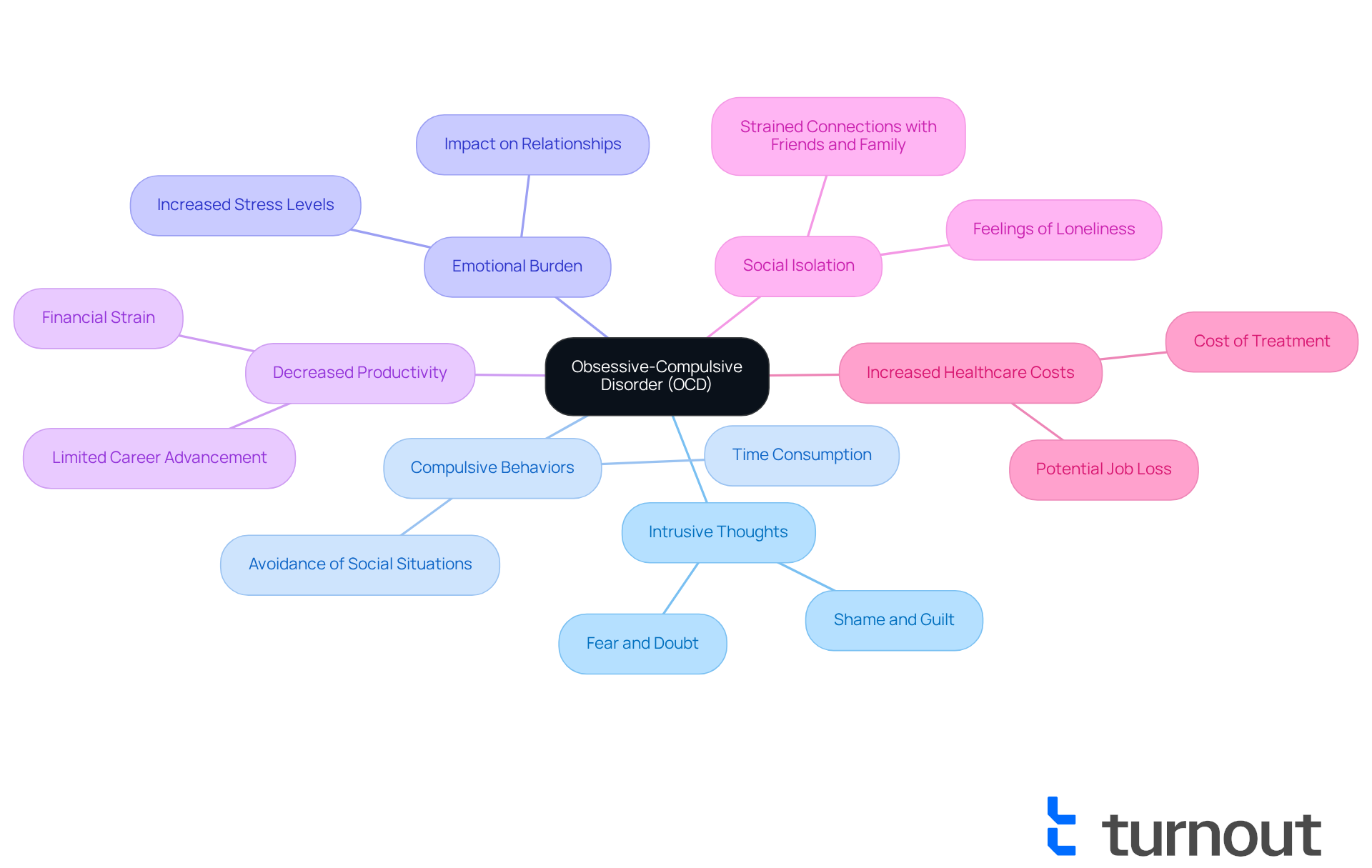
Obsessive-Compulsive Disorder (OCD) can feel overwhelming, marked by intrusive thoughts and compulsive behaviors that lead to significant anxiety. Many individuals with OCD find themselves dedicating hours each day to these compulsions, which raises the question of whether OCD is considered a disability, as it can disrupt work, academic performance, and personal relationships. For example, someone might avoid social gatherings due to fears of contamination, leading to feelings of isolation and strained connections with friends and family. This avoidance not only impacts the individual but also creates challenges for loved ones who may struggle to understand the complexities of the disorder.
The time-consuming nature of compulsions often results in decreased productivity. Studies show that the question of whether OCD is considered a disability can limit earning potential and career advancement opportunities. It's important to note that approximately 70% of individuals with OCD respond positively to exposure and response prevention therapy. This therapy can help individuals confront their fears and reduce compulsive behaviors, paving the way for a more fulfilling life. Additionally, the emotional burden of OCD can lead to heightened stress levels, complicating both personal and work-related challenges. This stress can contribute to increased healthcare costs and potential job loss, highlighting the broader implications of the disorder.
Recognizing these characteristics is essential for advocating for appropriate support and accommodations, particularly in discussions about whether OCD is considered a disability in various settings. We understand that seeking help can be daunting, but as Elizabeth McIngvale, founder of the Peace of Mind Foundation, emphasizes, reaching out to a mental health professional specializing in OCD is crucial for managing symptoms effectively. The challenges faced during the pandemic have further complicated the lives of those with OCD, as heightened health-related messaging has intensified compulsive behaviors.
As awareness of OCD grows, it becomes increasingly important to foster understanding among peers and employers. You are not alone in this journey, and ensuring that individuals affected by OCD receive the necessary resources to thrive is vital. Remember, we're here to help you navigate these challenges.
Conclusion
Understanding the complexities of Obsessive-Compulsive Disorder (OCD) is crucial in recognizing its profound impact on individuals' lives. We understand that living with OCD can be incredibly challenging, and this article delves into whether OCD qualifies as a disability under the Americans with Disabilities Act (ADA). By highlighting the significant challenges faced by those living with this condition, we aim to shed light on the emotional and functional limitations imposed by OCD. It becomes clear that this disorder can severely hinder daily activities, work performance, and personal relationships.
Key insights presented include:
- The prevalence of OCD
- The legal context surrounding disability rights
- The importance of effective treatment options like exposure and response prevention therapy
It's common to feel overwhelmed when seeking accommodations at work, and societal stigma often complicates the ability to advocate for oneself. We emphasize the necessity of fostering an inclusive environment that recognizes and supports the needs of those affected by OCD.
Ultimately, raising awareness and understanding of OCD not only empowers individuals to seek help but also encourages workplaces and communities to provide the necessary support. By promoting acceptance and dismantling misconceptions, society can create an environment where those with OCD can thrive. We believe it’s essential to ensure their rights are upheld and their challenges acknowledged. Let’s continue the conversation around OCD and disability rights, advocating for a future where everyone has access to the resources they need to lead fulfilling lives.
Frequently Asked Questions
What is Obsessive-Compulsive Disorder (OCD)?
Obsessive-Compulsive Disorder (OCD) is a long-lasting psychological condition characterized by persistent, unwanted thoughts known as obsessions, and repetitive actions or compulsions that individuals feel compelled to perform. These obsessions can lead to significant anxiety, while compulsions are often attempts to alleviate that anxiety or prevent a feared event.
How common is OCD?
OCD affects approximately 1% to 3% of the population, which translates to about 1 in 40 adults in the U.S.
Is OCD considered a disability?
OCD is often regarded as one of the most debilitating conditions, which can severely impact daily functioning, leading to isolation and hindering academic and career performance. This raises questions about its classification as a disability.
What are the emotional effects of untreated OCD?
The emotional toll of untreated OCD is profound, potentially leading to significant anxiety and affecting personal and social aspects of life.
What treatments are available for OCD?
Effective treatments for OCD include exposure and response prevention (ERP) therapy, which has shown considerable potential in helping individuals manage their symptoms. Mental health professionals note that ERP usually works better than medication in ideal circumstances.
How can individuals find support for OCD?
It is important for individuals struggling with OCD to seek the right support and treatment options. Awareness and effective treatment are crucial for managing the condition.




