Overview
Degenerative Disc Disease (DDD) can truly feel overwhelming. If it significantly impairs your ability to perform essential work tasks, it may be considered a disability under the Social Security Administration's criteria for spinal disorders. We understand that navigating this process can be challenging, and having comprehensive medical documentation is crucial. This evidence not only supports your case but also illustrates how DDD affects your daily activities.
It's important to recognize that symptoms can vary widely among individuals, impacting quality of life in different ways. You are not alone in this journey, and there are resources available to help you. Qualifying for disability benefits can provide much-needed support during difficult times. Remember, we're here to help you through this process, ensuring you have the guidance you need to advocate for yourself.
Introduction
Understanding the complexities of Degenerative Disc Disease (DDD) is crucial for millions who grapple with its effects on daily life. We recognize that this condition, characterized by the gradual breakdown of spinal discs, can lead to significant discomfort and mobility issues. This raises essential questions about its classification as a disability.
As individuals seek clarity on their eligibility for benefits and support, it becomes increasingly important to explore the nuances of DDD's impact on work and personal activities.
- What does it truly mean for someone to live with DDD?
- How can they navigate the maze of disability determination?
You're not alone in this journey, and we’re here to help guide you through.
Define Degenerative Disc Disease
Degenerative Disc Disease (DDD) is a condition that raises the question of whether degenerative disc disease is a disability for many people as they age or experience injury. It involves the gradual deterioration of the intervertebral discs in the spine, which serve as vital cushions between the vertebrae, offering essential support and flexibility. As these discs lose hydration and elasticity, discomfort and reduced mobility can arise, impacting daily life. While DDD is often viewed as a pathological condition, it frequently represents a natural part of aging, with severity varying widely among individuals. This variability can significantly affect daily activities and overall quality of life.
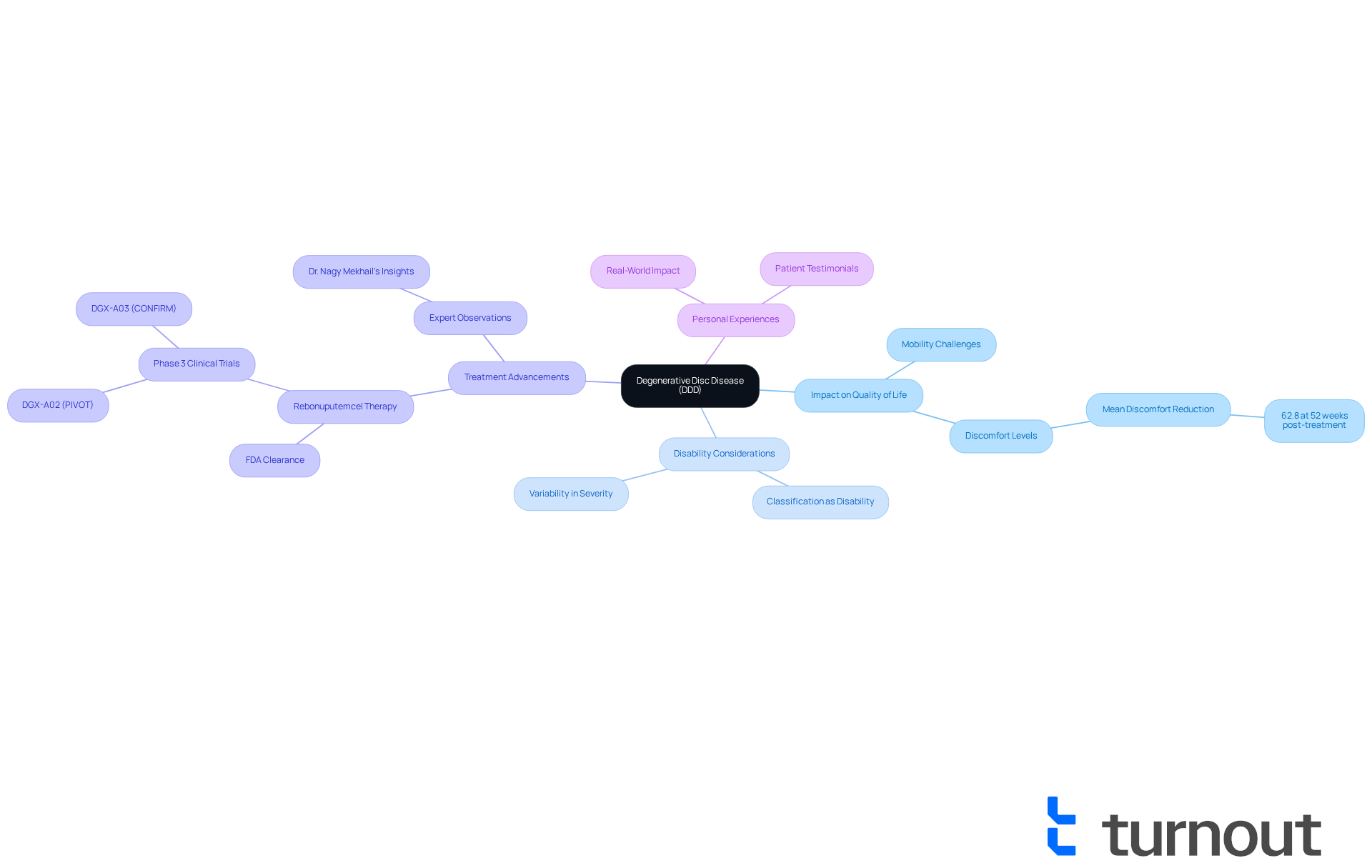
We understand that many people wonder if degenerative disc disease is a disability, as it affects millions of Americans each year, leading to persistent discomfort and mobility challenges. For instance, a previous phase 1/2 clinical trial demonstrated a mean discomfort reduction of 62.8% at 52 weeks post-treatment for patients receiving innovative therapies aimed at addressing DDD. Such findings highlight the importance of addressing the question of whether degenerative disc disease is a disability, viewing it not just as a medical issue, but as a crucial factor influencing the quality of life for many.
In light of recent advancements, DiscGenics has received FDA clearance to proceed with its phase 3 clinical program for its allogeneic discogenic progenitor cell therapy, rebonuputemcel, aimed at treating painful lumbar degenerative disc disease. Medical professionals emphasize the need for effective management strategies, especially when considering if degenerative disc disease is a disability. As Dr. Nagy Mekhail observes, there are few reliable treatments available for mechanical back pain, underscoring the promise of new therapies to transform care for individuals facing painful degenerative disc issues. Real-world examples show how DDD can significantly impact mobility, making daily activities challenging. Therefore, a comprehensive approach to treatment and support is essential. Remember, you are not alone in this journey, and we’re here to help.
Assess Disability Status of Degenerative Disc Disease
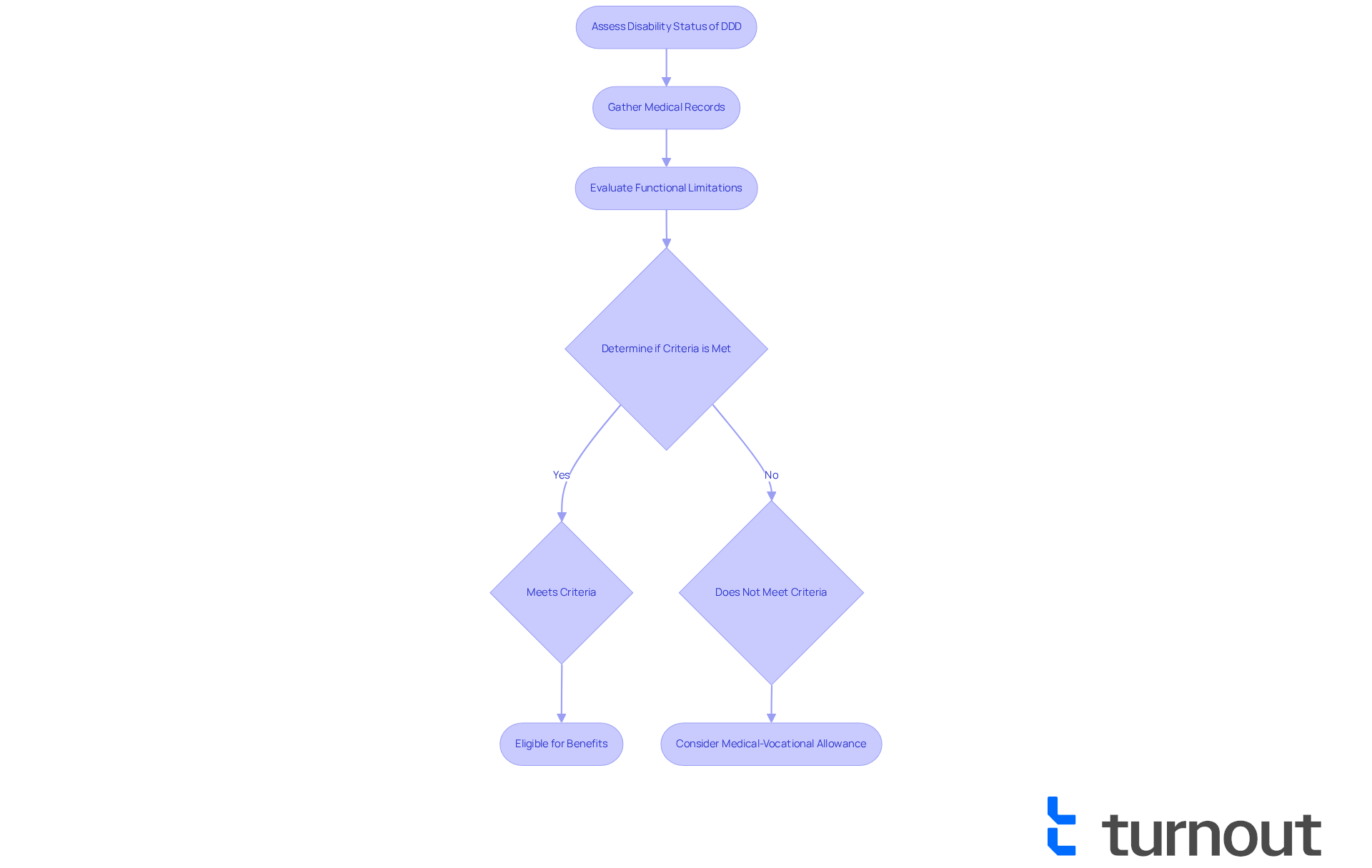
Understanding whether degenerative disc disease is a disability can be overwhelming. We recognize that navigating this process is not easy, but we're here to help. The Social Security Administration (SSA) has specific evaluation criteria, and DDD is included in their Listing of Impairments under section 1.04, which outlines the requirements for spinal disorders. If DDD significantly obstructs your ability to perform essential work tasks, one might wonder, is degenerative disc disease a disability?
The SSA evaluates the seriousness of your situation through comprehensive medical records, including imaging studies and treatment history. Chronic pain, restricted mobility, and other functional limitations can hinder your ability to work productively. If you find yourself in this situation, you may be eligible for disability benefits. It’s important to submit thorough medical evidence to support your claims, as this documentation is crucial for a successful application.
Recent cases have shown that individuals with DDD who provide comprehensive medical histories and illustrate how their health affects daily activities have had their claims accepted. If your condition doesn’t meet the formal criteria but still significantly limits your daily activities, you might qualify for a 'medical-vocational allowance.'
Living with degenerative disc disease is challenging enough without questioning if degenerative disc disease is a disability in the complex benefits system. That’s why Turnout offers tools and services to assist you through this process. Our trained nonlegal advocates are here to guide you through the SSD claims procedure. Remember, persistence and thoroughness in your application can make a difference. You are not alone in this journey, and support is available to help you every step of the way.
Identify Symptoms and Challenges of Degenerative Disc Disease
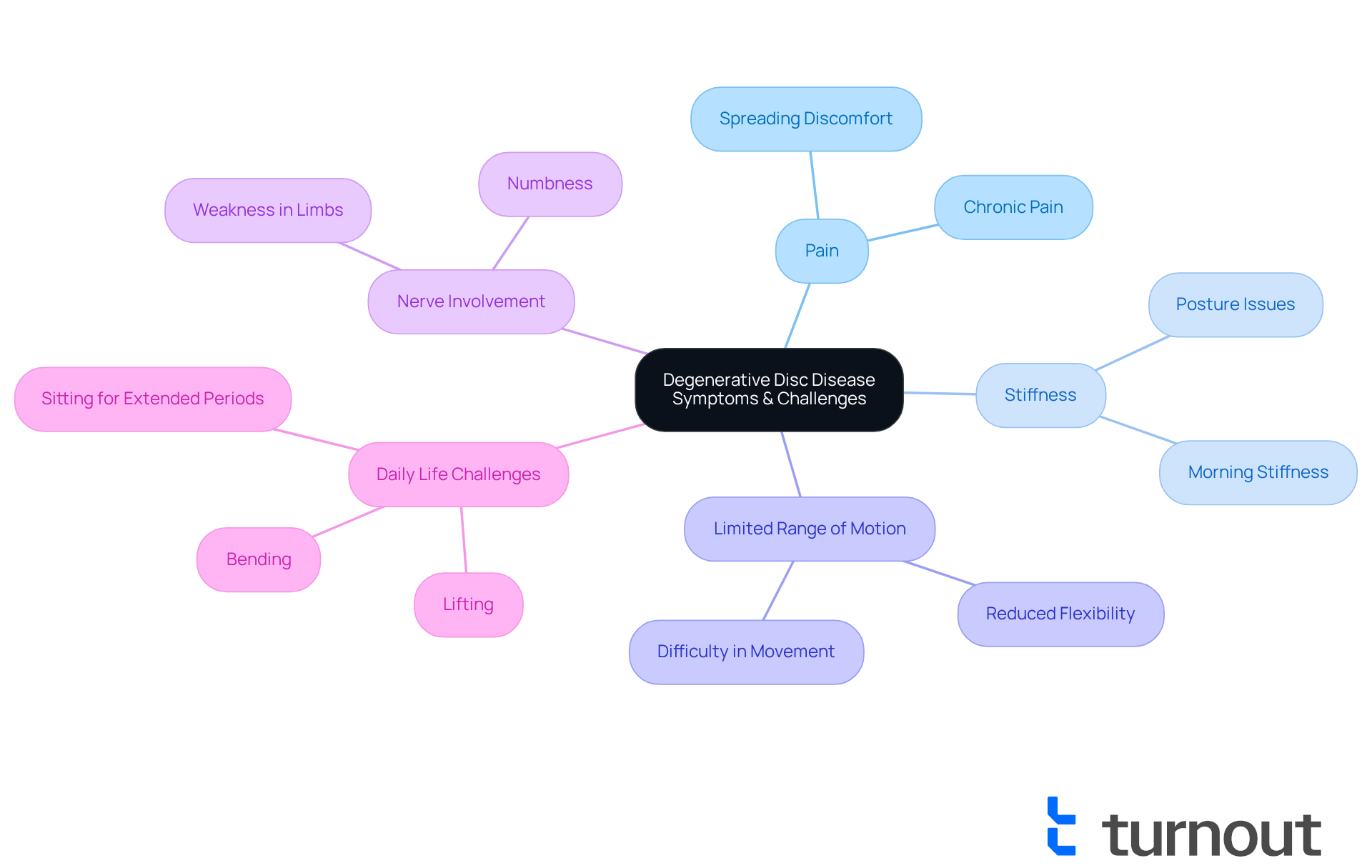
Symptoms of Degenerative Disc Disease (DDD) can manifest in various ways, often leading to persistent back discomfort, stiffness, and a limited range of motion. Many individuals experience spreading discomfort, numbness, or weakness in their limbs, particularly when nerve roots are involved. These symptoms can create significant challenges in daily activities—lifting, bending, or sitting for extended periods can become daunting tasks. It's common to feel overwhelmed by the unpredictable nature of flare-ups, which can disrupt both work and personal life.
We understand that the challenges faced by those with DDD can lead to the consideration of whether degenerative disc disease is a disability, as they can greatly hinder routine tasks, resulting in increased frustration and emotional distress. It's important to recognize that you are not alone in this journey. Statistics reveal that chronic pain affects millions, with conditions like osteoarthritis impacting 27 million Americans, highlighting the widespread nature of mobility challenges.
Understanding whether degenerative disc disease is a disability is vital for advocating for necessary accommodations and benefits. By doing so, we ensure that individuals receive the support they need to navigate their circumstances effectively. Remember, we're here to help you through this process.
Explore Diagnosis and Treatment Options for Degenerative Disc Disease
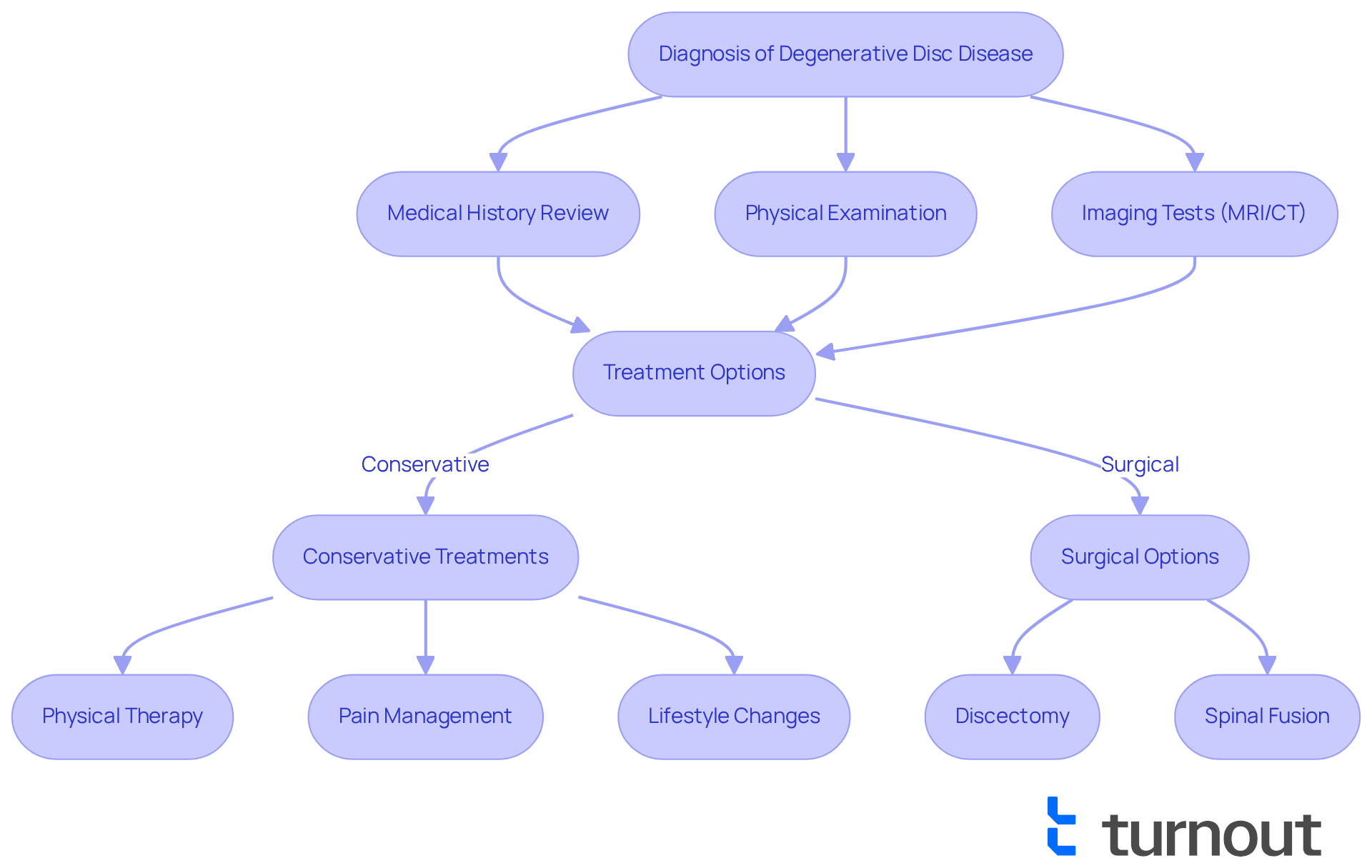
Diagnosing Degenerative Disc Disease (DDD) can feel overwhelming, but understanding the process can bring some relief. It typically involves a detailed review of your medical history, a physical examination, and imaging tests such as MRI or CT scans to evaluate disc degeneration and any nerve compression.
In 2025, there are diverse treatment options available for DDD, tailored to the severity of your condition. Conservative methods often include:
- Physical therapy
- Pain management techniques
- Lifestyle changes aimed at enhancing mobility and alleviating discomfort
For those experiencing significant symptoms, surgical options like discectomy or spinal fusion may be necessary to relieve pain and restore function.
Many treatment plans for DDD patients begin with non-invasive approaches. For example, you might start with a regimen of physical therapy that focuses on strengthening your core muscles and improving flexibility, combined with pain management strategies such as medication or injections. If these methods do not provide enough relief, your healthcare provider may recommend surgical intervention based on your specific circumstances.
Medical professionals stress the importance of a personalized treatment plan. As one expert observes, 'Each patient's experience with Degenerative Disc Disease is unique, and treatment should be customized to their specific symptoms and lifestyle requirements.' This collaborative approach ensures that you receive the most effective care, enhancing your quality of life as you navigate the challenges posed by DDD.
We understand that ongoing developments in healthcare, including advancements in treatment methodologies and patient advocacy tools, are crucial for improving outcomes for individuals with DDD. Remember, you are not alone in this journey; we're here to help you find the best path forward.
Conclusion
Degenerative Disc Disease (DDD) presents a complex interplay between physical health and the potential for disability status. This condition, characterized by the deterioration of spinal discs, can significantly impact mobility and quality of life. It's common to feel uncertain about whether it qualifies as a disability. Understanding the nuances of DDD is crucial for individuals navigating its challenges, as it can influence access to necessary support and benefits.
Throughout this article, we’ve shared key insights regarding the diagnosis, symptoms, and treatment options for DDD. We also discussed the criteria set by the Social Security Administration for determining disability eligibility. The importance of comprehensive medical documentation and advocacy cannot be overstated. Those whose daily lives are profoundly affected by this condition can find hope in knowing that persistence in presenting one’s case can lead to successful claims for disability support.
Ultimately, recognizing the impact of Degenerative Disc Disease is essential not only for individuals seeking assistance but also for raising awareness about the broader implications of this condition. As advancements in treatment continue to evolve, it is vital to stay informed and proactive in seeking the care and support you need. Remember, you are not alone in this journey, and resources are available to help you navigate toward improved health and well-being.
Frequently Asked Questions
What is Degenerative Disc Disease (DDD)?
Degenerative Disc Disease (DDD) is a condition characterized by the gradual deterioration of the intervertebral discs in the spine, which serve as cushions between the vertebrae. This deterioration can lead to discomfort and reduced mobility, impacting daily life.
Is Degenerative Disc Disease considered a disability?
Many people wonder if DDD is a disability, as it affects millions of Americans and can lead to persistent discomfort and mobility challenges. The severity of DDD varies widely among individuals, and it can significantly affect quality of life.
How does aging affect Degenerative Disc Disease?
DDD is often viewed as a natural part of aging. As individuals age, their intervertebral discs may lose hydration and elasticity, leading to discomfort and reduced mobility.
What recent advancements have been made in treating DDD?
DiscGenics has received FDA clearance to proceed with its phase 3 clinical program for its allogeneic discogenic progenitor cell therapy, rebonuputemcel, aimed at treating painful lumbar degenerative disc disease.
What are the challenges in managing Degenerative Disc Disease?
There are few reliable treatments available for mechanical back pain associated with DDD. Effective management strategies are essential for improving the quality of life for individuals facing this condition.
How does DDD impact daily activities?
DDD can significantly impact mobility, making daily activities challenging for those affected. A comprehensive approach to treatment and support is necessary to address these challenges.




