Introduction
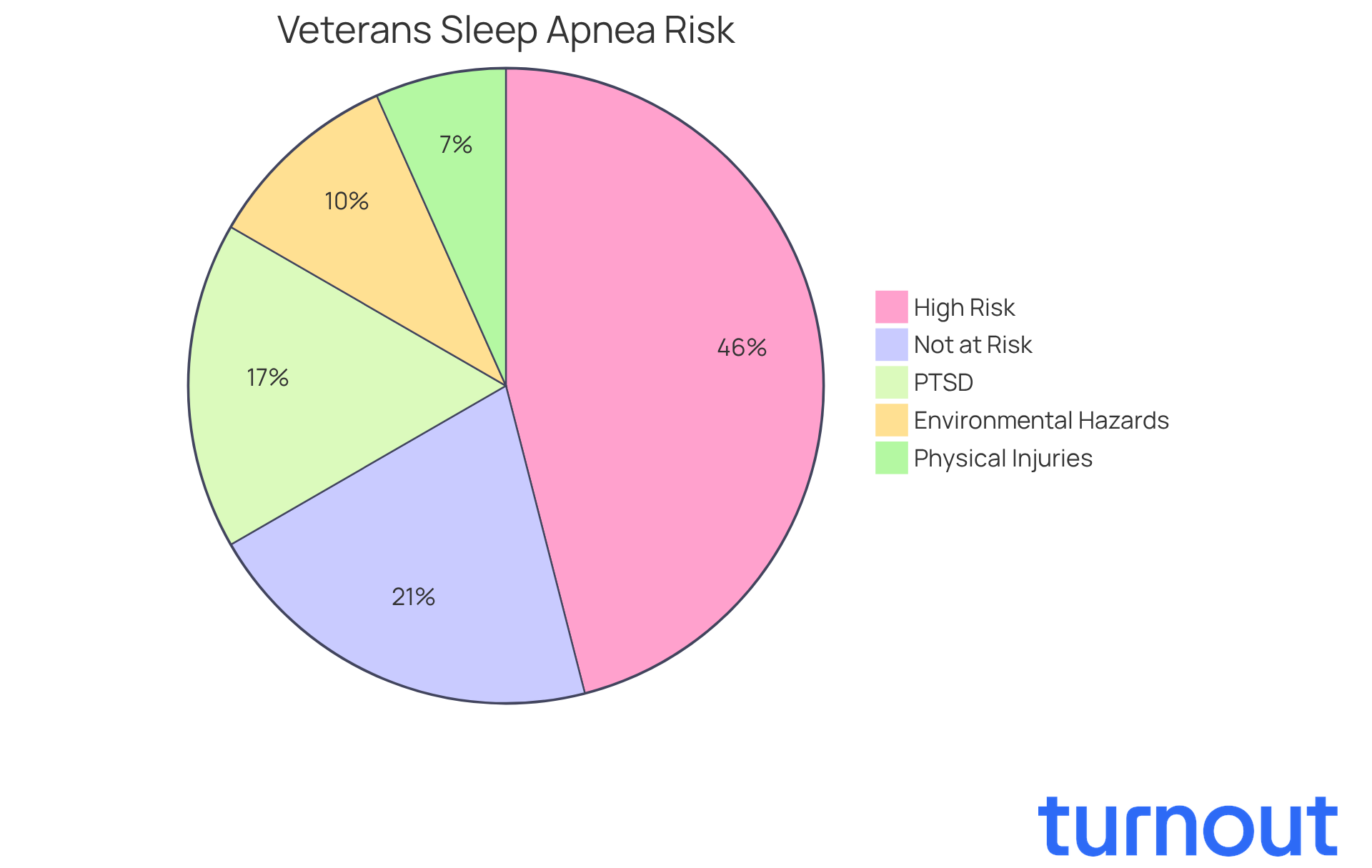
Breathing disorders during sleep are a serious concern for veterans. Did you know that nearly 69 percent of younger veterans are at high risk for conditions like sleep apnea? This statistic is alarming and highlights the importance of understanding the impact of this condition. Sleep apnea doesn’t just affect physical health; it also intertwines with mental health issues, including PTSD.
We understand that navigating the complexities of establishing a service connection for sleep apnea can be overwhelming. Veterans often face the challenge of gathering the right documentation and evidence to support their claims. It’s common to feel lost in this process. How can you effectively bridge the gap between your military service and this debilitating condition to secure the benefits you deserve?
You are not alone in this journey. We’re here to help you find the support you need.
Understand Sleep Apnea and Its Impact on Veterans
Breathing disorders during rest can be a serious concern, especially for veterans. Did you know that around 69 percent of younger veterans are at a high risk for these conditions? This is significantly higher than the general population. Factors like exposure to environmental hazards during service, physical injuries, and mental health issues such as PTSD contribute to this risk. In fact, more than half of veterans diagnosed with obstructive breathing disorders also struggle with PTSD.
Recognizing symptoms is crucial. Loud snoring, gasping for air during sleep, and excessive daytime fatigue are all signs that shouldn’t be ignored. We understand that acknowledging these symptoms can be difficult, but doing so is essential. It not only helps in seeking timely medical intervention but also supports your case for VA disability benefits. This establishes the need for treatment and support.
Many veterans who have started continuous positive airway pressure (CPAP) therapy report feeling better and less fatigued. Imagine waking up refreshed and ready to face the day! Addressing this condition can significantly improve your quality of life. Remember, you are not alone in this journey. We're here to help you navigate these challenges and find the support you need.
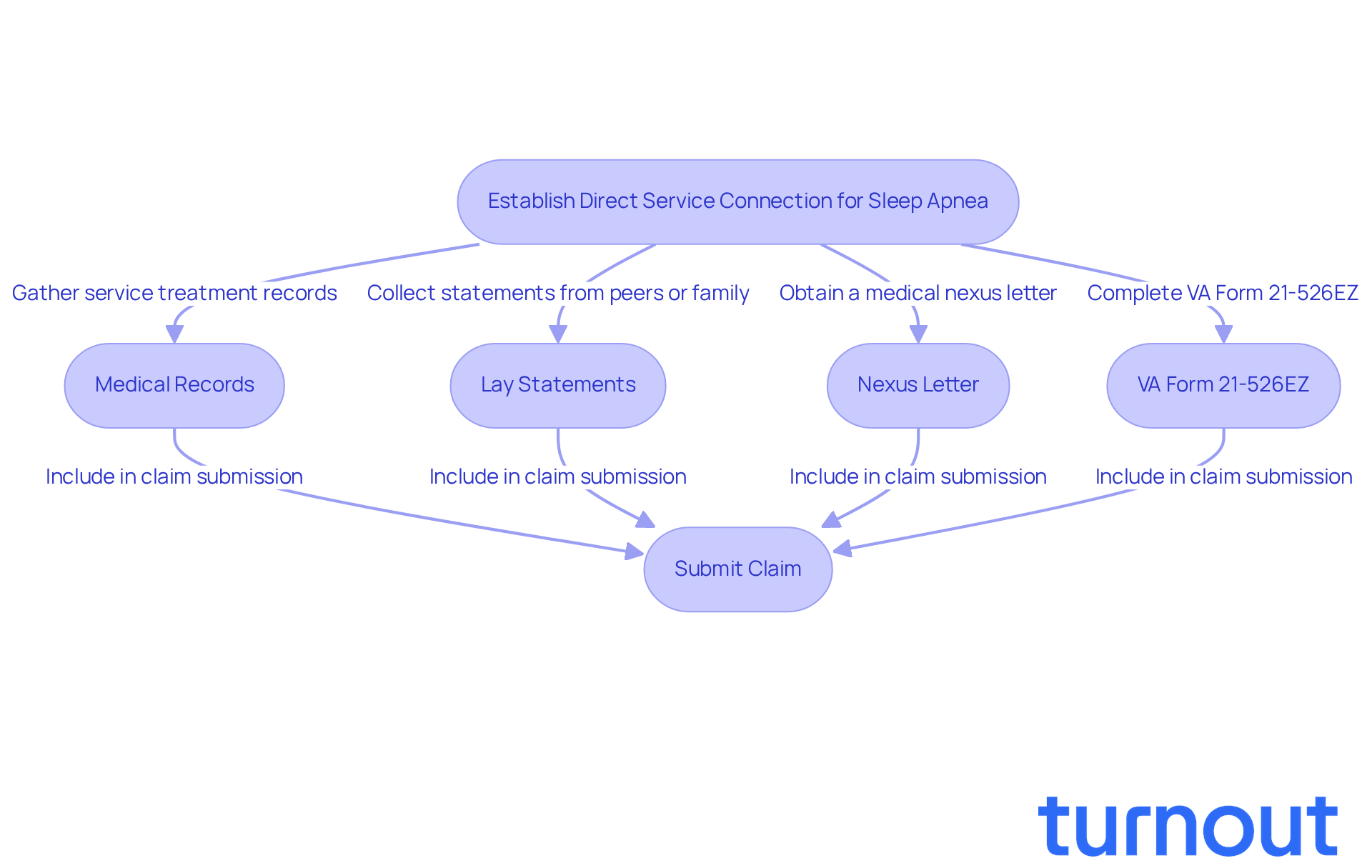
Establish Direct Service Connection for Sleep Apnea
Veterans need to know how to service connect sleep apnea for obstructed breathing during rest by providing compelling evidence that their condition began or was diagnosed during active duty. We understand that this process can feel overwhelming, but gathering the right documentation can make a significant difference. Here are some key components to consider:
-
Medical Records: Secure your service treatment records that document any complaints or diagnoses related to sleep disorders during your military service. These records are vital, as they provide a timeline and context for your condition. It’s important to note that veterans are three to four times more likely to be diagnosed with a sleep disorder than civilians, highlighting the need for thorough documentation.
-
Lay Statements: Gather statements from fellow service members or family members who can attest to your symptoms during service. Individual accounts can enhance the credibility of your claim by demonstrating how disrupted rest has affected your daily life.
-
Nexus Letter: Obtain a medical nexus letter from a qualified healthcare provider that connects your condition to your military service. This letter should detail how specific service conditions contributed to your condition, reinforcing the connection. As Brian Reese, creator of VA Claims Insider, emphasizes, "If you haven't submitted your rest disorder request yet, do it now." Once the new criteria take effect, securing a 50% rating will be much harder-if not impossible.
-
VA Form 21-526EZ: Complete and submit this form to initiate your request, ensuring that your condition is clearly mentioned as the issue being reported. This form is essential for processing your application.
By gathering extensive evidence, you can effectively demonstrate how to service connect sleep apnea to your military service, greatly enhancing your chances of a successful application. Given that this condition is one of the most frequently rejected VA requests, comprehensive documentation is crucial for navigating the complexities of the application process. Furthermore, with anticipated changes to VA ratings for respiratory disorders expected before the end of 2025, it’s vital to submit claims under the current system. Remember, you are not alone in this journey, and we’re here to help.
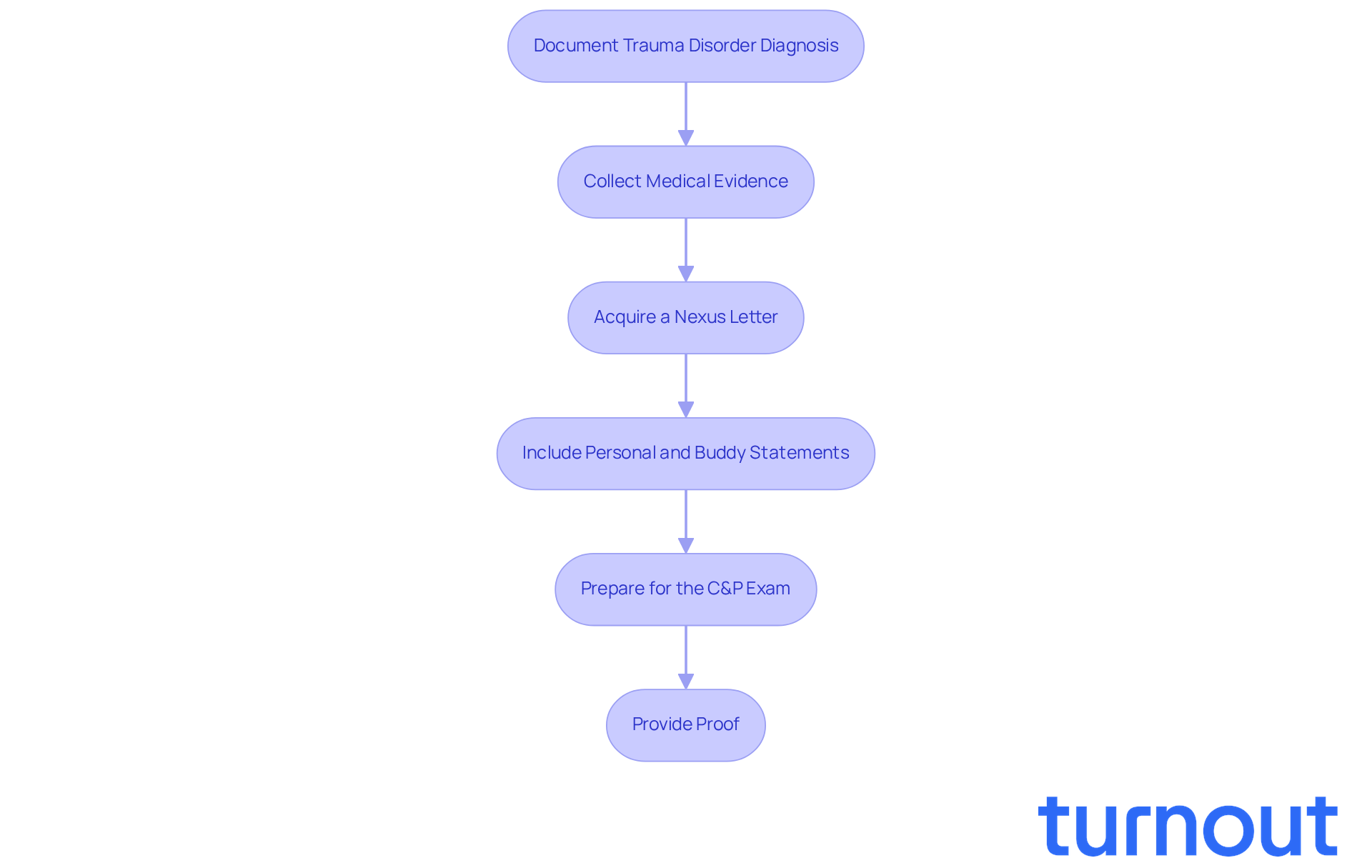
Connect Sleep Apnea as a Secondary Condition to PTSD
Veterans often face a challenging link between disrupted sleep and post-traumatic stress disorder (PTSD), stemming from their service-related trauma. If you or someone you know is navigating this difficult path, here are some steps to help you make your case:
-
Document Trauma Disorder Diagnosis: Start by obtaining a formal diagnosis of trauma disorder from a qualified mental health professional. This is a crucial first step in understanding your condition.
-
Collect Medical Evidence: Gather medical documents that illustrate how trauma-related symptoms - like anxiety and hyperarousal - can lead to sleep disturbances. Research shows that veterans with PTSD are at a significantly higher risk for obstructive sleep issues. In fact, studies indicate that 69% of Iraq and Afghanistan veterans receiving treatment for PTSD are at high risk for these problems.
-
Acquire a Nexus Letter: It’s important to get a nexus letter from your healthcare provider. This letter should clearly outline how to service connect sleep apnea by detailing the connection between your PTSD and sleep difficulties, and explaining how your trauma exacerbates breathing issues at night.
-
Include Personal and Buddy Statements: Consider adding personal statements and buddy statements. These can provide valuable insights into how your sleep disorder relates to your PTSD, helping to paint a fuller picture.
-
Prepare for the C&P Exam: Be ready for the Compensation and Pension (C&P) exam. This evaluation will assess how your breathing difficulties and PTSD affect your daily life. Bring along any personal sleep study records, as they can serve as essential evidence for your claim.
-
Provide Proof: When you submit your request, make sure to include all relevant paperwork using VA Form 21-526EZ. This form indicates that you are asserting a connection between insomnia and PTSD.
By clearly establishing this connection, you can enhance your chances of qualifying for VA benefits, even if there isn’t a direct service link for your condition. This approach not only boosts the likelihood of a successful claim but also highlights how to service connect sleep apnea in the context of the complex relationship between mental health and sleep issues. Remember, you are not alone in this journey, and we’re here to help you navigate the VA system.
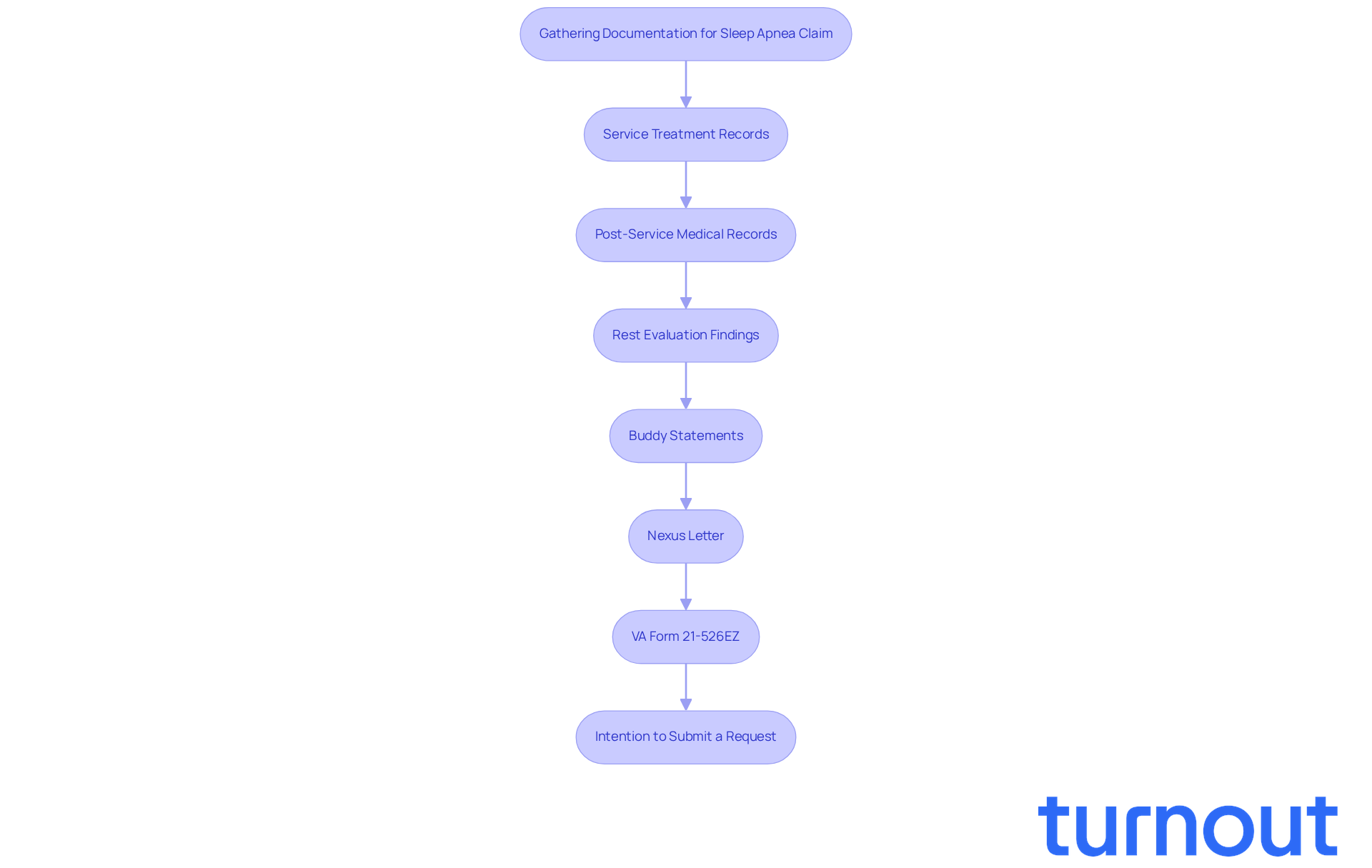
Gather Essential Documentation and Evidence for Your Claim
Filing a claim for sleep apnea can feel overwhelming, but you’re not alone in this journey. To successfully navigate this process, it’s essential to gather comprehensive documentation and evidence. Here’s what you need:
- Service Treatment Records: These records should detail any sleep-related complaints or diagnoses made during your service. They help establish a direct link to your military experience.
- Post-Service Medical Records: Include records from VA or private healthcare providers that document your insomnia diagnosis and treatment. This shows continuity of care, which is crucial.
- Rest Evaluation Findings: An official diagnosis of breathing interruptions during rest often requires outcomes from a rest evaluation (polysomnography). This is vital for validating your claim.
- Buddy Statements: Collect statements from friends or family who can attest to your symptoms and their impact on your daily life. Their personal insights can significantly support your case.
- Nexus Letter: If you’re asserting a secondary service connection, make sure you have a nexus letter linking your sleep disorder to PTSD or another service-related condition. A well-crafted nexus letter can greatly enhance your claim, as legal experts emphasize.
- VA Form 21-526EZ: Complete this form accurately, listing all claimed conditions and attaching all supporting documents. This ensures a thorough submission.
- Intention to Submit a Request: If you’re still gathering evidence, consider submitting an Intention to Submit a Request using VA form 21-0966. This can secure an effective date for your request.
We understand that compiling all necessary documentation can be daunting, but it is important to learn how to service connect sleep apnea, as doing so can significantly enhance your chances of a successful claim. Requests backed by thorough evidence have shown greater approval rates. Statistics reveal that veterans with robust supporting documentation succeed in their applications at much higher rates.
It’s crucial to avoid filing without adequate documentation, as this can lead to delays or denials. The time to act is now-delaying your claim could cost you thousands in benefits if the proposed changes to the VA rating system take effect. Remember, we’re here to help you through this process.
Conclusion
Navigating the complexities of service connection for sleep apnea is crucial for veterans seeking the benefits they deserve. We understand that many veterans face significant challenges, especially those suffering from PTSD, where the prevalence of sleep apnea is notably high. Addressing this condition is not just important; it’s essential for your health and well-being.
In this guide, we’ve outlined key strategies to help you establish a service connection for sleep apnea. From gathering essential medical documentation and lay statements to securing nexus letters, each step plays a vital role in strengthening your claim. Remember, thorough evidence collection is paramount, especially with the anticipated changes to VA rating systems by 2025.
Ultimately, addressing sleep apnea goes beyond securing benefits; it’s about reclaiming your quality of life. You deserve the support you need, and taking action now can prevent future complications and enhance your overall health. If you’re navigating this process, know that resources and assistance are available to help you every step of the way. You are not alone in this journey.
Frequently Asked Questions
What is sleep apnea and why is it a concern for veterans?
Sleep apnea is a breathing disorder that occurs during rest, and it is a significant concern for veterans due to a high prevalence of these conditions among them, with around 69 percent of younger veterans at a high risk.
What factors contribute to the high risk of sleep apnea in veterans?
Factors contributing to the high risk include exposure to environmental hazards during service, physical injuries, and mental health issues such as PTSD.
How does PTSD relate to sleep apnea in veterans?
More than half of veterans diagnosed with obstructive breathing disorders also struggle with PTSD, indicating a strong connection between the two conditions.
What are the common symptoms of sleep apnea that veterans should recognize?
Common symptoms include loud snoring, gasping for air during sleep, and excessive daytime fatigue.
Why is it important for veterans to acknowledge symptoms of sleep apnea?
Acknowledging symptoms is crucial for seeking timely medical intervention and can support a veteran's case for VA disability benefits, establishing the need for treatment and support.
What treatment is commonly used for sleep apnea, and what benefits does it provide?
Continuous positive airway pressure (CPAP) therapy is commonly used, and many veterans report feeling better and less fatigued after starting this treatment.
How can addressing sleep apnea improve a veteran's quality of life?
Addressing sleep apnea can significantly improve a veteran's quality of life by allowing them to wake up refreshed and ready to face the day, reducing fatigue and enhancing overall well-being.
Where can veterans seek support for sleep apnea?
Veterans can seek support through medical professionals and resources available to help navigate the challenges associated with sleep apnea.




