Introduction
Understanding the relationship between sleep apnea and various secondary conditions is crucial for veterans looking to improve their health and secure necessary benefits. Many former military personnel face challenges like anxiety, PTSD, and obesity, all linked to sleep apnea. Recognizing these connections can open important pathways to better disability ratings and support.
We understand that navigating these issues can feel overwhelming. It’s common to wonder how these conditions intertwine and what steps you can take to ensure your claims reflect the full extent of your health challenges.
You are not alone in this journey. We're here to help you understand the importance of these connections and how they can impact your well-being. By acknowledging your struggles and seeking the right support, you can take meaningful steps toward improving your health.
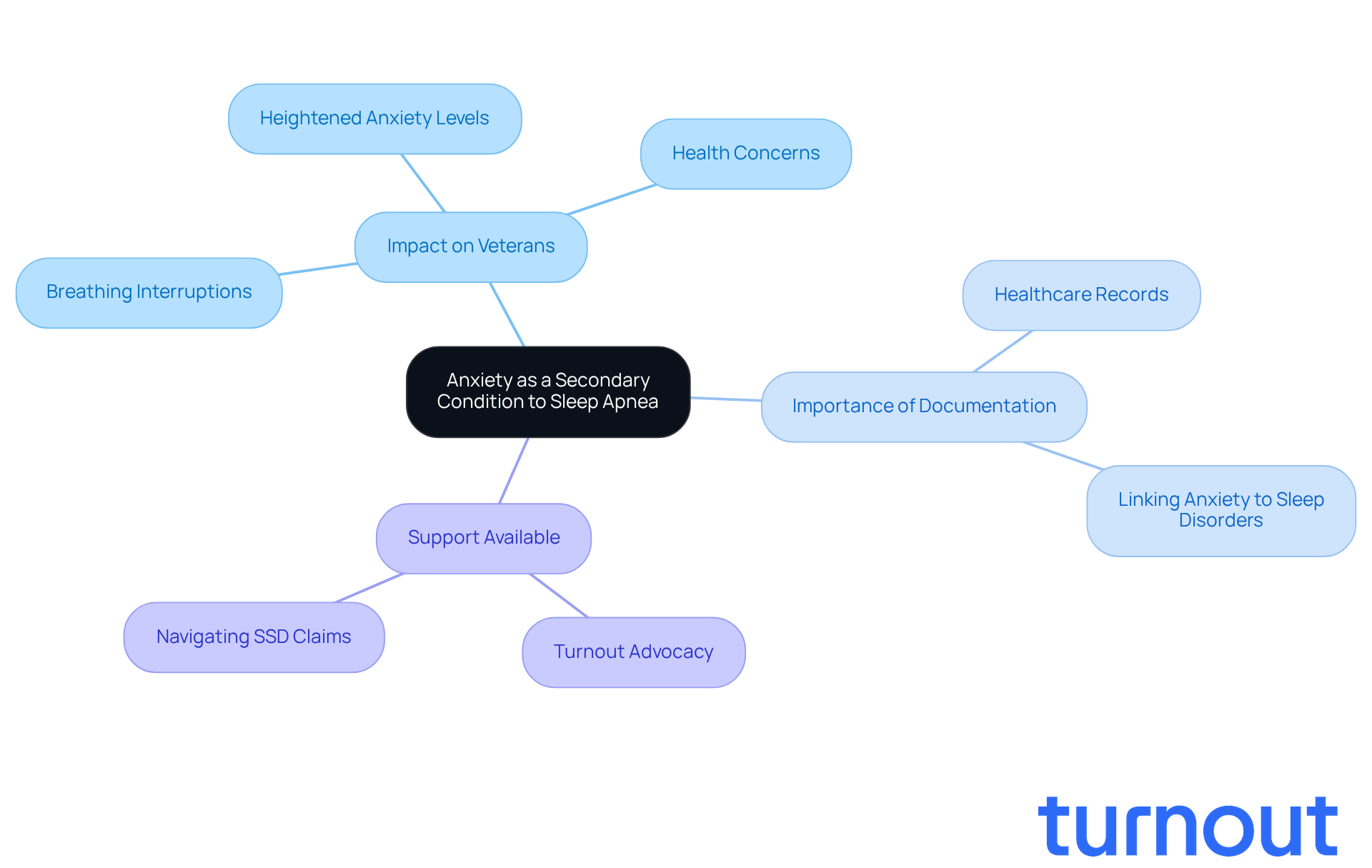
Anxiety as a Secondary Condition to Sleep Apnea
Anxiety disorders are all too common among former military personnel, especially those who experience breathing interruptions during rest. These issues often stem from the stress and fear linked to disrupted sleep patterns. We understand that this can lead to heightened anxiety levels, which may worsen overall health concerns.
For many ex-servicemen diagnosed with sleep disorders, anxiety often accompanies these challenges. This highlights how interconnected these issues can be. Recognizing anxiety as one of the VA secondary conditions to sleep apnea is crucial for veterans seeking VA benefits, as it can potentially improve their disability rating.
To strengthen their claims, former service members should gather comprehensive records from healthcare professionals that clearly link their anxiety to breathing disorders during rest. This documentation can significantly enhance their chances of receiving the benefits they deserve.
At Turnout, we’re here to help navigate these complexities. Our trained nonlawyer advocates are dedicated to assisting veterans with their SSD claims, ensuring they receive the support they need. Remember, you are not alone in this journey.
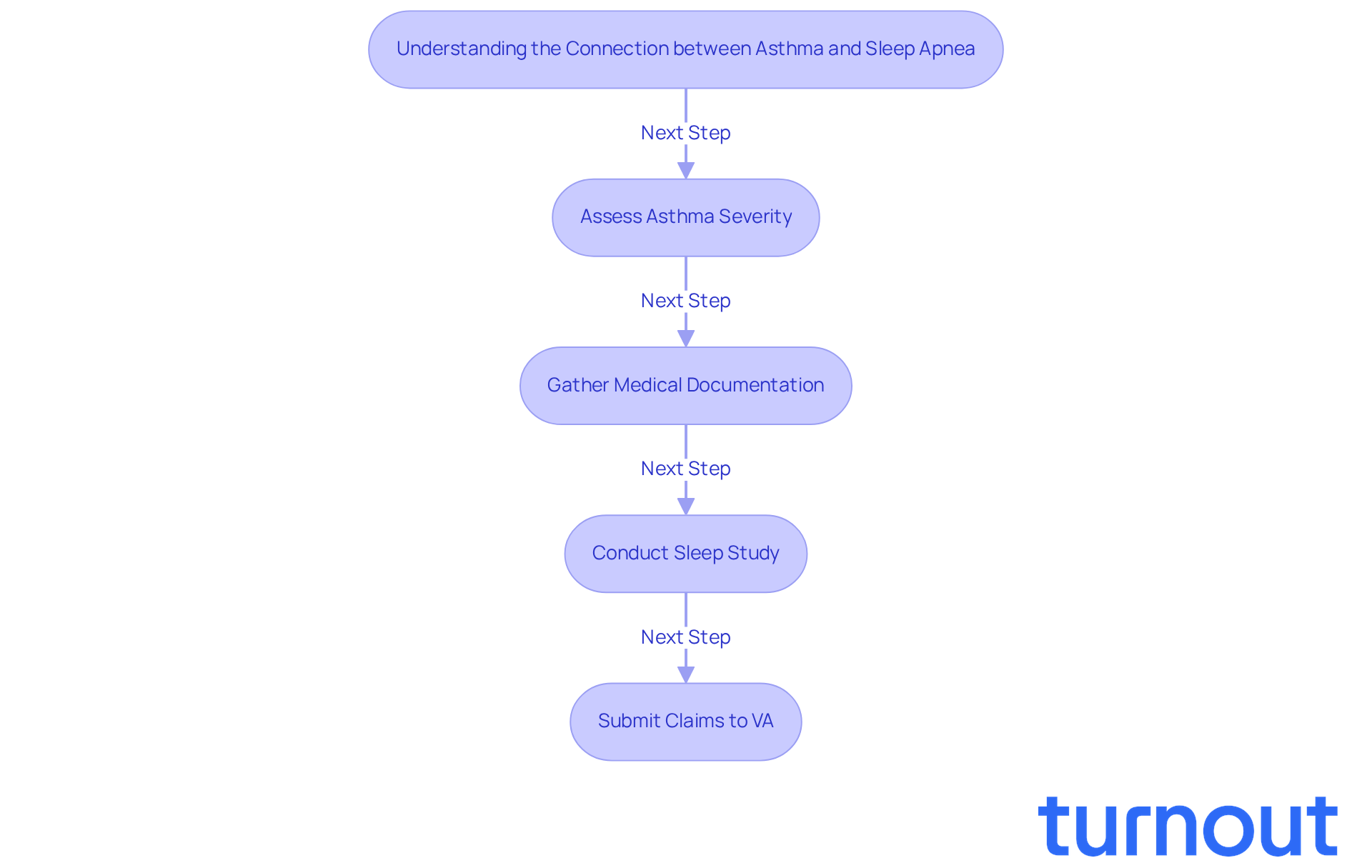
Asthma Linked to Sleep Apnea
Asthma and nighttime breathing issues often go hand in hand, and we understand how challenging this can be. These breathing interruptions can worsen asthma symptoms, leading to increased airway inflammation. It’s concerning to know that individuals with asthma face nearly a 40% higher risk of developing obstructive breathing issues compared to those without asthma.
This connection is particularly significant for former military personnel. The VA acknowledges the impact of respiratory issues on asthma and recognizes the importance of VA secondary conditions to sleep apnea by allowing for additional benefits requests. To navigate the claims process effectively, veterans need to provide thorough documentation of their asthma severity and its relationship to breathing interruptions during rest. This evidence is crucial for establishing VA secondary conditions to sleep apnea.
Moreover, a sleep study is essential to confirm a diagnosis of a sleep disorder for VA disability compensation. This highlights the importance of comprehensive medical documentation. As pulmonologists note, managing asthma in patients with breathing interruptions requires careful attention to both conditions to optimize treatment outcomes.
Remember, you are not alone in this journey. We’re here to help you through the process and ensure you receive the support you need.
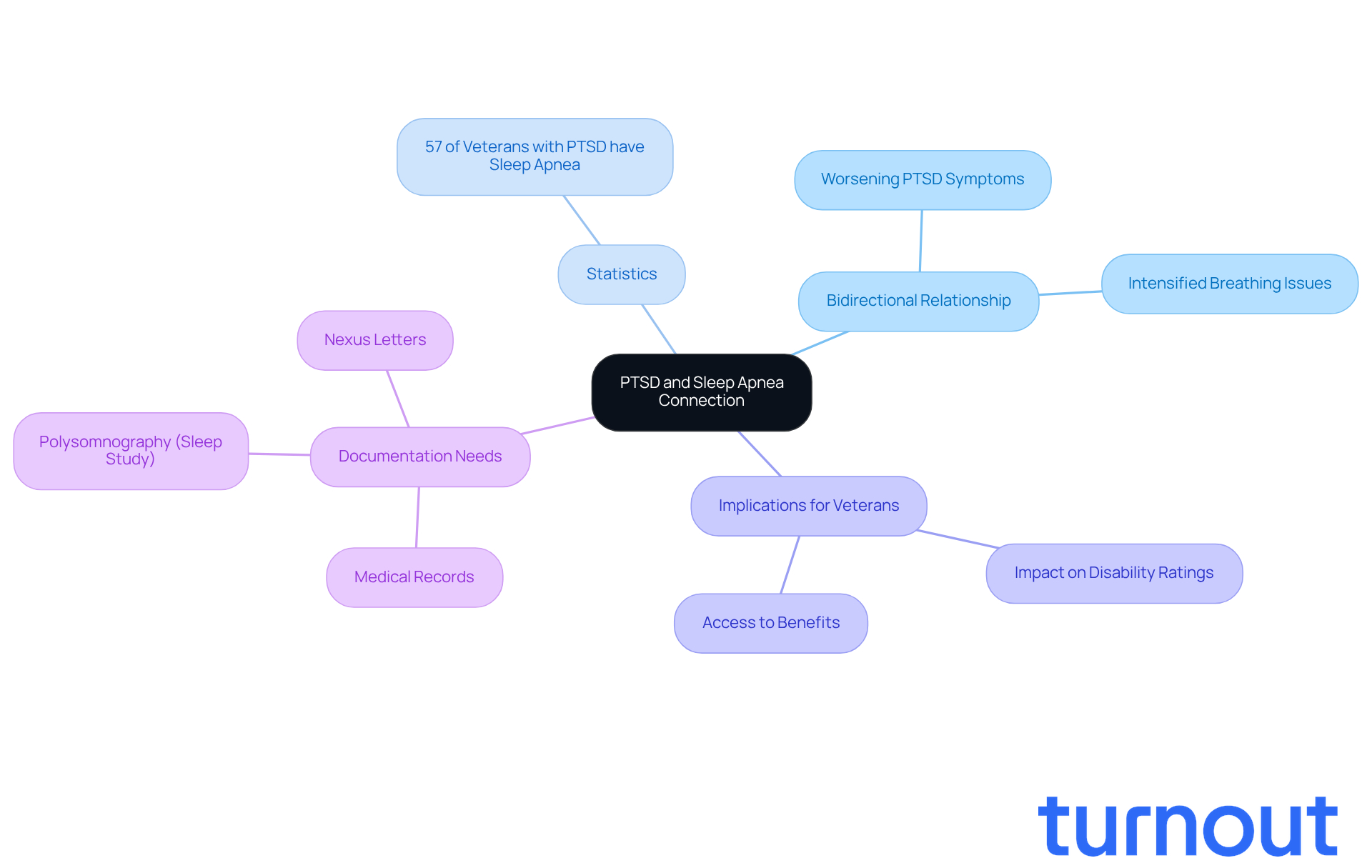
Post-Traumatic Stress Disorder as a Secondary Condition to Sleep Apnea
The connection between Post-Traumatic Stress Disorder (PTSD) and breathing interruptions during rest is particularly significant for former military personnel. We understand that the stress and anxiety associated with PTSD can deeply affect the quality of rest. Current research highlights a bidirectional relationship: interrupted breathing can worsen PTSD symptoms, while the distress from PTSD can intensify breathing issues. This cycle can lead to increased daytime fatigue, irritability, and difficulty concentrating, complicating overall well-being.
Did you know that over 57% of individuals diagnosed with PTSD also have VA secondary conditions to sleep apnea? This statistic underscores the commonality of this dual diagnosis. For veterans, the implications are profound. The link between these VA secondary conditions to sleep apnea can significantly impact disability ratings and access to benefits. It’s crucial for veterans to ensure their requests accurately reflect this relationship. Thorough documentation-comprising medical records, study results, and personal accounts-can strengthen their case for compensation.
Furthermore, a polysomnography (rest study) is essential to confirm eligibility for compensation related to disrupted breathing stemming from PTSD. By addressing their claims related to VA secondary conditions to sleep apnea, former service members can better advocate for the support they deserve. Remember, you are not alone in this journey; we’re here to help you navigate these challenges.
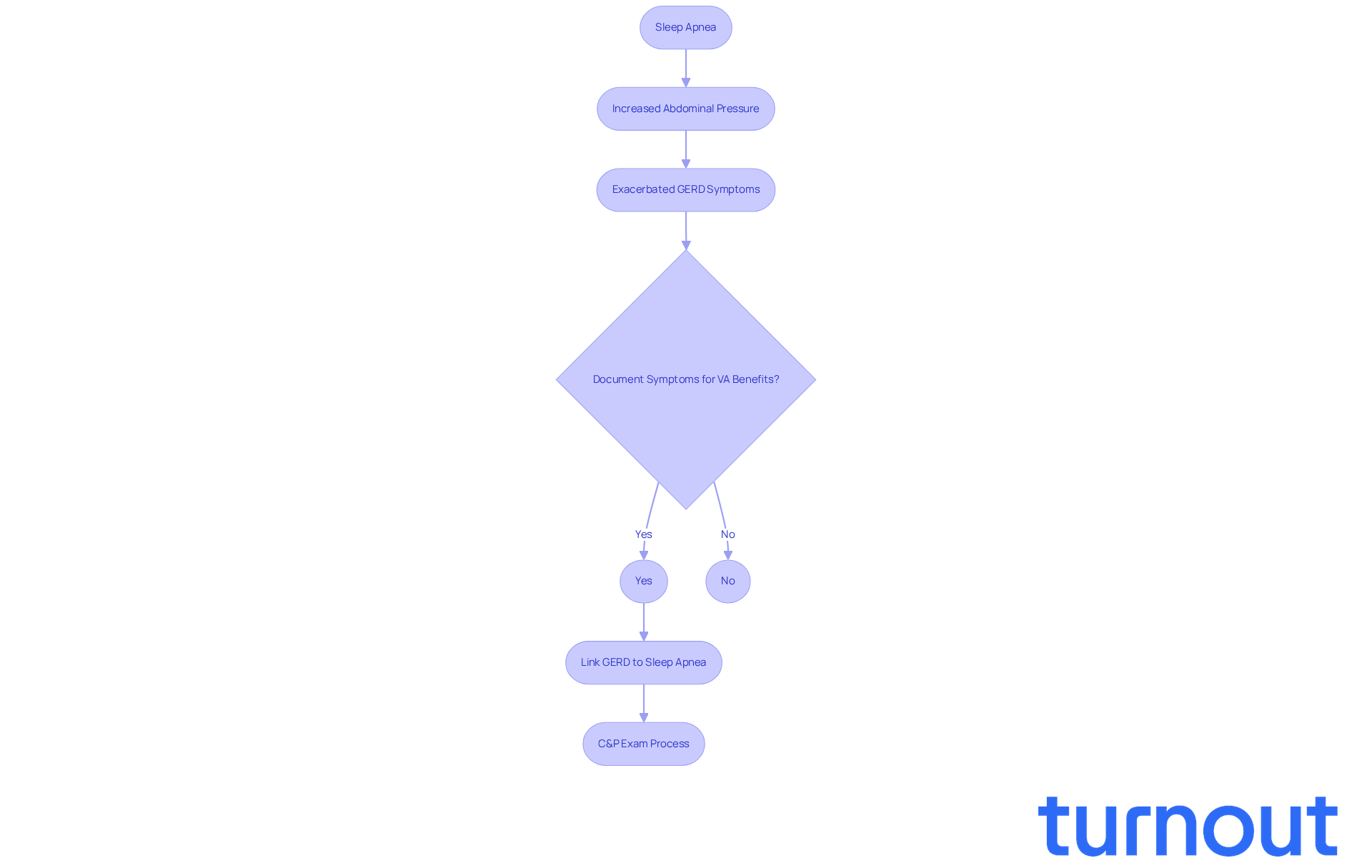
Gastroesophageal Reflux Disease (GERD) Secondary to Sleep Apnea
Gastroesophageal Reflux Disease (GERD) can be a challenging companion for many, especially for veterans who experience breathing interruptions during rest. This often happens due to increased abdominal pressure during apneic episodes, which can intensify reflux symptoms. We understand that this can lead to significant discomfort and potential health issues. Research indicates that former service members with breathing difficulties at rest are more likely to develop GERD, as airway blockages can exacerbate the condition. For example, studies reveal that:
- 47 percent of patients with PTSD struggle to maintain rest, while
- 41 percent find it hard to initiate it.
This can complicate GERD symptoms even further.
When applying for VA benefits, it’s crucial for veterans to document their GERD symptoms and clearly link them as VA secondary conditions to sleep apnea related to their insomnia. This careful documentation can greatly strengthen their claims, as establishing a medical nexus between the two conditions is vital for service connection. Gastroenterologists emphasize the importance of recognizing this connection. They note that unaddressed nighttime breathing issues can worsen GERD symptoms, such as heartburn, regurgitation, and difficulty swallowing. As April Donahower wisely points out, 'If the individual has previously been diagnosed with sleep apnea, but has not undergone a sleep study, the VA will not consider that diagnosis as sufficient evidence for verifying eligibility for compensation related to VA secondary conditions to sleep apnea.'
We encourage veterans to actively discuss these symptoms with their healthcare providers. This proactive approach ensures comprehensive care and support throughout the claims process. Additionally, understanding the Compensation and Pension (C&P) exam process is essential. This exam assesses the severity and cause of the veteran's condition and its connection to the primary disability. Remember, you are not alone in this journey, and we’re here to help.
Hypothyroidism as a Secondary Condition to Sleep Apnea
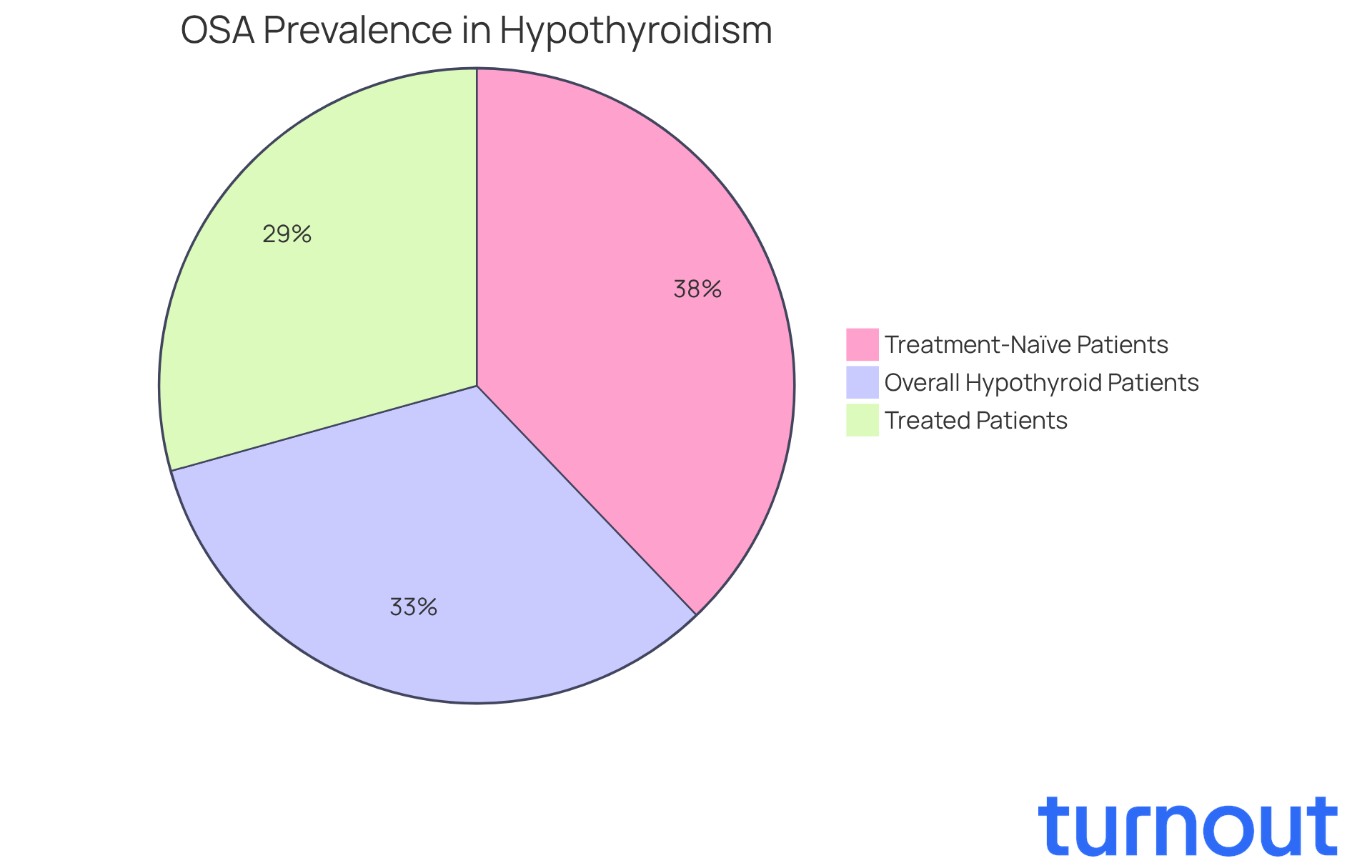
Hypothyroidism can significantly impact breathing interruptions during rest, often leading to changes in the upper airway that may worsen symptoms. We understand that this can be concerning. Recent research indicates that untreated hypothyroidism is linked to a greater severity of obstructive breathing interruptions. For instance, a staggering 74% of hypothyroid patients were diagnosed with obstructive sleep apnea (OSA), highlighting how prevalent this condition is in this demographic. Moreover, treatment-naïve patients showed an even higher prevalence of OSA at 85.3%, compared to 66.1% in those undergoing treatment. This suggests that effectively managing hypothyroidism may help reduce the severity of nocturnal breathing disorders.
Veterans, in particular, should prioritize assessments that evaluate thyroid function. Understanding the relationship between hypothyroidism and nighttime breathing disorders, particularly as secondary conditions to sleep apnea, is crucial for their disability claims. It's common to feel overwhelmed by these health concerns, especially as the average age of individuals with OSA tends to be higher among those with hypothyroidism. This underscores the need for specialized screening in older individuals.
Furthermore, the connection between thyroid hormone levels and the severity of obstructive respiratory events is still being explored. Evidence shows that lower free T4 levels and higher TSH levels are often found in individuals with OSA. This highlights the importance of early identification and treatment of both conditions, particularly as secondary conditions to sleep apnea, to minimize potential health complications. Remember, you are not alone in this journey, and seeking help can make a significant difference.
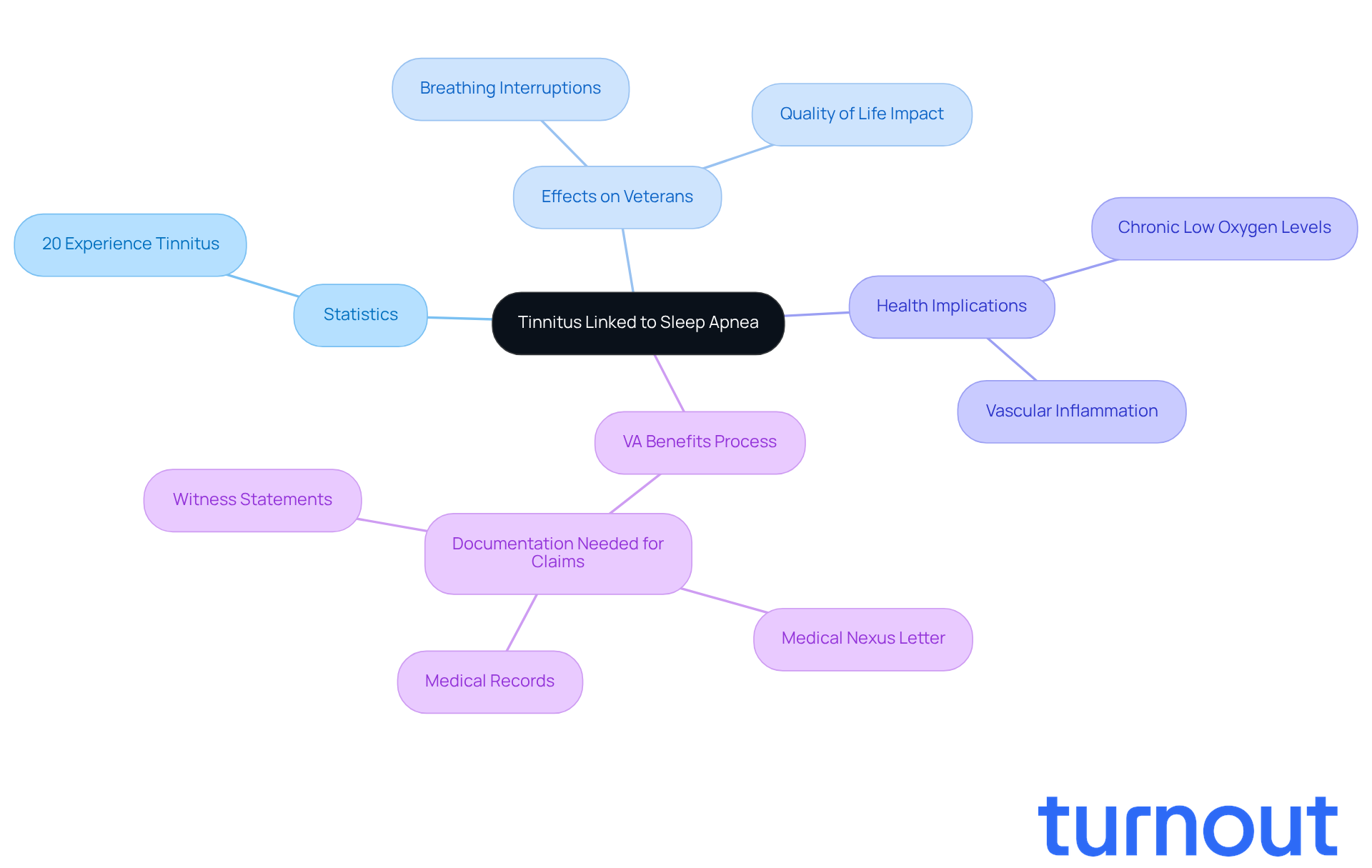
Tinnitus Linked to Sleep Apnea
Tinnitus is a challenge many face, especially those who have served in the military. We understand that breathing interruptions during rest can be particularly distressing. Recent studies suggest that these interruptions, often linked to hypoxia, may worsen or even trigger tinnitus. Did you know that around 20% of people experience tinnitus at some point in their lives? This figure is especially significant for veterans dealing with obstructive breathing issues, who might experience anywhere from one to 100 interruptions per hour while resting.
Chronic low oxygen levels can harm the delicate cochlear hair cells in the inner ear over time, potentially leading to tinnitus. Research shows that former service members with breathing disturbances during rest are more likely to report that ringing in their ears. This can greatly affect daily activities and overall quality of life. Moreover, nighttime breathing disruptions can cause vascular inflammation, which may hinder blood circulation to auditory structures, complicating the relationship between these conditions.
It's essential for veterans to document their tinnitus symptoms and how they relate to VA secondary conditions to sleep apnea when applying for VA benefits. This careful record-keeping can significantly enhance their applications. If you have been diagnosed with both conditions, we encourage you to seek a service connection for VA secondary conditions to sleep apnea. This could help you secure a higher VA disability rating.
When submitting your VA claim for tinnitus related to breathing difficulties, remember to include a medical nexus letter, medical records, and witness statements. These elements are crucial for a successful claim. You're not alone in this journey, and we're here to help you navigate the process.
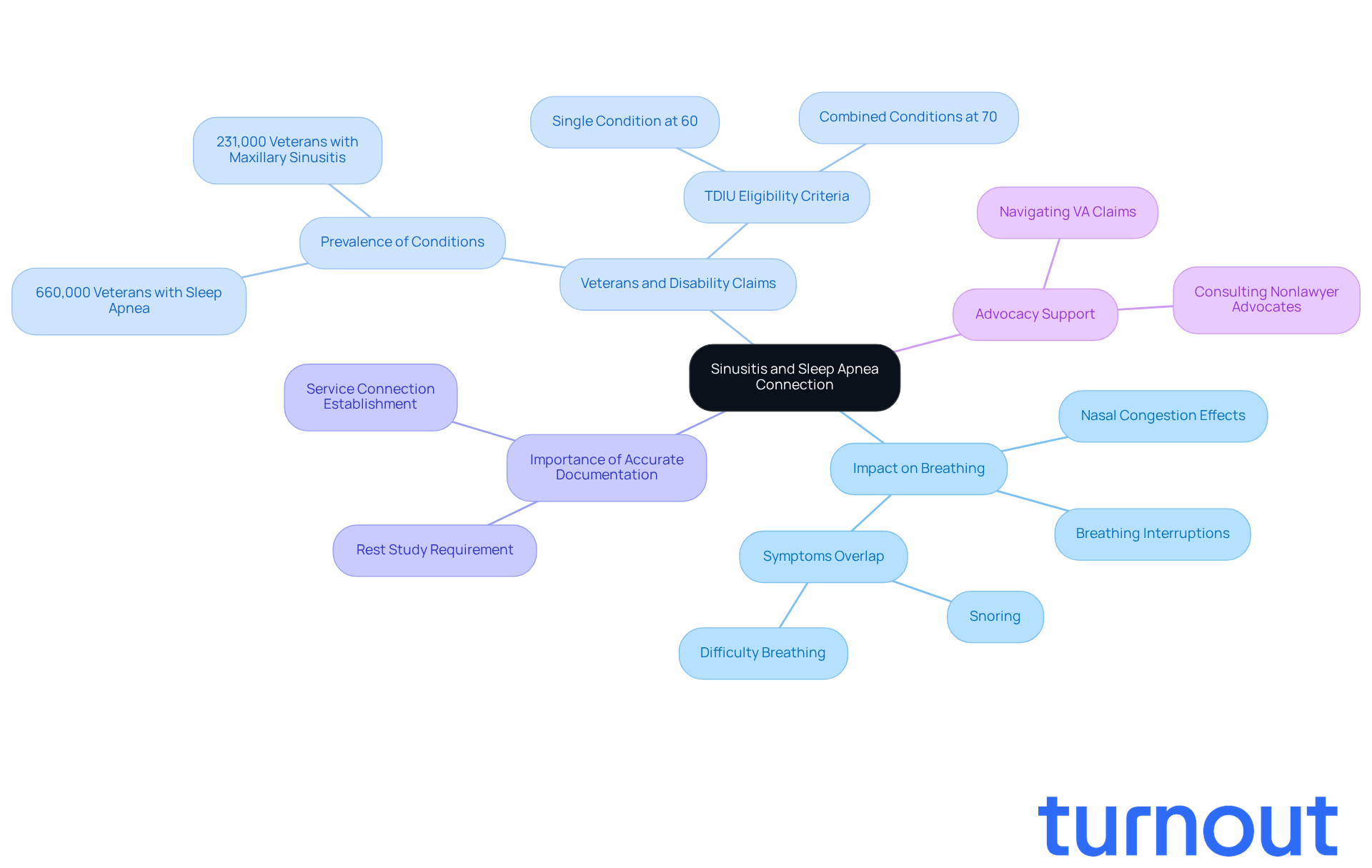
Sinusitis as a Secondary Condition to Sleep Apnea
Sinusitis can lead to nasal congestion, making it hard to breathe comfortably, especially during rest. This connection is particularly significant for veterans. Untreated sinusitis can severely affect the quality of rest and overall health. Chronic sinusitis, characterized by prolonged inflammation and swelling of the sinuses, can complicate nighttime breathing, increasing the likelihood of breathing interruptions.
Veterans, it’s crucial to ensure that your disability claims accurately reflect any diagnoses of sinusitis and its link to respiratory issues, particularly the VA secondary conditions to sleep apnea, during rest. This step can enhance your chances of qualifying for benefits. Did you know that around 660,000 former service members currently receive disability compensation for respiratory issues? This makes it the second-most common breathing disorder among VA disability beneficiaries.
Establishing a clear connection between VA secondary conditions to sleep apnea is essential. It may help you qualify for VA secondary conditions to sleep apnea, which can significantly influence your overall disability rating and access to benefits. To strengthen your claims, we encourage you to consult with Turnout's trained nonlawyer advocates. They can assist in ensuring that all necessary documentation, including a rest study confirming the diagnosis of sleep conditions, is included.
It's important to remember that Turnout is not a law firm and does not provide legal advice. However, they offer valuable support in navigating the complexities of government benefits without needing legal representation. You're not alone in this journey, and we're here to help.
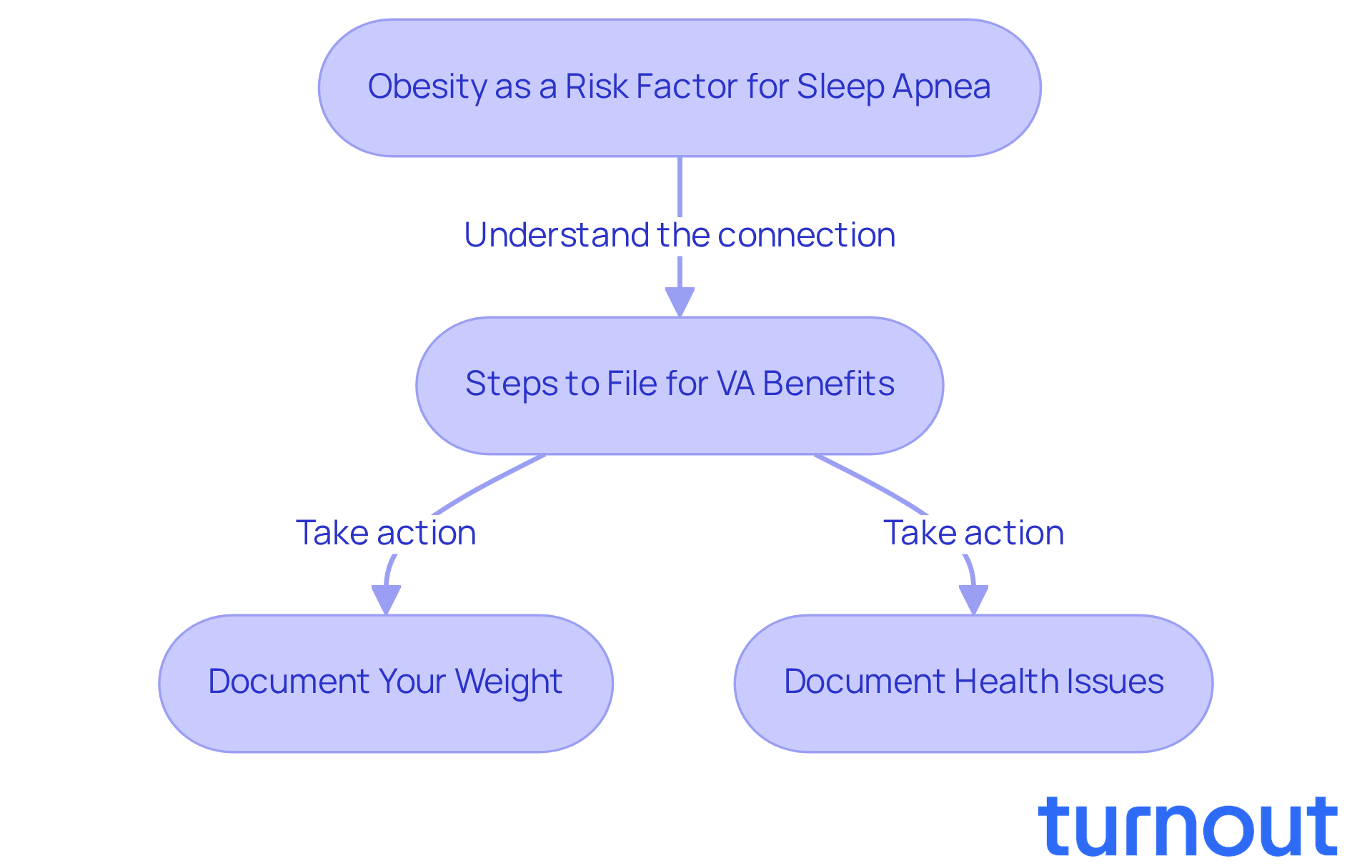
Obesity as a Secondary Condition to Sleep Apnea
Obesity can be a significant risk factor for sleep apnea, as excess weight often leads to airway obstruction during sleep. We understand that this connection is particularly relevant for veterans, many of whom may struggle with weight management due to various factors, including medication side effects.
It's common to feel overwhelmed by these challenges. However, there are steps you can take to address them. When filing for VA benefits, veterans should:
- Document their weight
- Document any health issues, particularly VA secondary conditions to sleep apnea
This important information can enhance your claims and ensure you receive the support you deserve.
Remember, you are not alone in this journey. We're here to help you navigate these challenges and advocate for your health.
Depression Linked to Sleep Apnea
Depression often affects those who experience breathing interruptions during rest. We understand that these disturbances can lead to significant mood changes and cognitive challenges. Research shows that untreated respiratory issues not only trigger depression but can also worsen existing symptoms.
For veterans, this connection is particularly important. Did you know that breathing interruptions during rest impact nearly 1 in 4 men and 1 in 10 women in middle age? This issue is especially prevalent among veterans, often due to factors like obesity and PTSD. It’s crucial for veterans to ensure their requests accurately reflect this relationship, as it can significantly influence their disability rating and access to essential benefits.
The VA recognizes depression as a secondary condition to sleep apnea. Acquiring a medical nexus letter that connects the two is vital for a successful request. This letter should clearly outline how respiratory issues have contributed to or intensified the service member's depression. Remember, thorough medical records play a key role in the claims process.
You are not alone in this journey. We’re here to help you navigate these challenges and ensure you receive the support you deserve.
Understanding the Importance of Recognizing Secondary Conditions to Sleep Apnea
It is crucial for former military personnel seeking VA benefits to identify VA secondary conditions to sleep apnea that are linked to breathing-related nighttime disorders. We understand that many veterans may not realize how conditions like anxiety, depression, and obesity can be considered VA secondary conditions to sleep apnea, intertwining with their breathing difficulties during rest. This connection can significantly impact their overall health and eligibility for benefits.
Research shows that about 14% of adults with obstructive sleep apnea report experiencing anxiety symptoms. Additionally, obesity - a recognized risk factor for sleep apnea - continues to rise among former military personnel. It's common to feel overwhelmed by these challenges, but recognizing them is the first step toward better health.
Importantly, the VA can assess secondary conditions independently and include them in the total disability rating. This can enhance an individual's application and improve their chances of receiving the support they need. Comprehensive assessments and detailed records from healthcare providers are essential for navigating the compensation process effectively.
Veterans must demonstrate that their illness or injury is service-connected to qualify for disability benefits. Therefore, we encourage you to discuss all health issues with your providers. This proactive approach can lead to a more accurate assessment of your conditions and ensure you receive the necessary support.
Understanding the relationship between sleep apnea and VA secondary conditions to sleep apnea can strengthen a veteran's claim. By addressing these interconnected issues, you may find yourself on the path to increased benefits and an improved quality of life. Remember, you are not alone in this journey; we're here to help.
Conclusion
Understanding the connections between sleep apnea and various secondary conditions is crucial for veterans looking to enhance their health and secure the benefits they deserve. The relationships among conditions like:
- anxiety
- asthma
- PTSD
- GERD
- hypothyroidism
- tinnitus
- sinusitis
- obesity
- depression
show just how deeply sleep apnea can affect overall well-being. Recognizing these links can significantly impact a veteran's disability rating and access to essential support.
Throughout this article, we've shared key insights about how these secondary conditions aren't merely coexisting issues; they often intertwine with the challenges posed by sleep apnea. For example, anxiety and depression can worsen sleep disturbances, while conditions like asthma and GERD may be aggravated by interrupted breathing during sleep. Each of these relationships underscores the importance of thorough documentation and proactive communication with healthcare providers to strengthen claims for VA benefits.
Ultimately, addressing sleep apnea and its secondary conditions is about more than just navigating the claims process; it’s about enhancing quality of life. Veterans are encouraged to take action by discussing their symptoms with healthcare professionals and ensuring that all relevant health issues are documented. By understanding and advocating for these interconnected conditions, veterans can pave the way for better health outcomes and greater support from the VA. Remember, assistance is available, and you are not alone in this journey toward improved health and well-being.
Frequently Asked Questions
How is anxiety related to sleep apnea in veterans?
Anxiety disorders are common among veterans, particularly those experiencing breathing interruptions during sleep. This connection highlights how anxiety can exacerbate health issues related to sleep apnea.
Why is it important for veterans to recognize anxiety as a secondary condition to sleep apnea?
Recognizing anxiety as a secondary condition to sleep apnea is crucial for veterans seeking VA benefits, as it can potentially improve their disability rating.
What should veterans do to strengthen their claims for anxiety related to sleep apnea?
Veterans should gather comprehensive medical records from healthcare professionals that clearly link their anxiety to breathing disorders during rest, as this documentation can enhance their chances of receiving benefits.
What is the relationship between asthma and sleep apnea?
Asthma and nighttime breathing issues often co-occur, with breathing interruptions worsening asthma symptoms and increasing airway inflammation. Individuals with asthma face a higher risk of developing obstructive breathing issues.
How can veterans document the connection between asthma and sleep apnea for VA benefits?
Veterans need to provide thorough documentation of their asthma severity and its relationship to breathing interruptions during rest to establish VA secondary conditions to sleep apnea.
What role does a sleep study play in obtaining VA disability compensation for sleep disorders?
A sleep study is essential to confirm a diagnosis of a sleep disorder, which is necessary for VA disability compensation related to sleep apnea.
How does Post-Traumatic Stress Disorder (PTSD) relate to sleep apnea in veterans?
There is a significant connection between PTSD and breathing interruptions during sleep, where interrupted breathing can worsen PTSD symptoms, and PTSD distress can intensify breathing issues.
What percentage of individuals with PTSD also have sleep apnea as a secondary condition?
Over 57% of individuals diagnosed with PTSD also have VA secondary conditions to sleep apnea, highlighting the commonality of this dual diagnosis.
What documentation is needed for veterans to support their claims related to PTSD and sleep apnea?
Veterans should provide thorough documentation, including medical records, study results, and personal accounts, to strengthen their case for compensation related to PTSD and sleep apnea.
How can veterans get support in navigating claims related to sleep apnea and its secondary conditions?
Organizations like Turnout offer assistance through trained nonlawyer advocates who help veterans navigate the complexities of their SSD claims and ensure they receive the support they need.




